Translate this page into:
Successful management of a rare arteriovenous malformation associated with scar ectopic pregnancy through uterine artery embolization: A case report in interventional radiology
* Corresponding author: Ankit Shah, Department of Radiodiagnosis, Gandhi medical College, Bhopal, India. ankitshah.md04@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Shah A, Kaushal L. Successful management of a rare arteriovenous malformation associated with scar ectopic pregnancy through uterine artery embolization: A case report in interventional radiology. Future Health. 2024;2:82–86. doi: 10.25259/FH_17_2024
Abstract
Arteriovenous malformation (AVM) may manifest in Cesarean scar ectopic pregnancy. The diagnostic challenge arises when retained products of conception are present, leading to a clinical presentation similar to that of a raised beta-human chorionic gonadotropin (HCG) titre, necessitating the exclusion of neoplastic etiology. Interventional Radiology (IR) opinion and uterine artery embolization stand as a treatment alternative to hysterectomy in such cases.
A 26-year-old female presented with continuous vaginal bleeding persisting for 16–18 days following a pharmacological termination of pregnancy. She had a history of three previous Cesarean sections. Color Doppler imaging revealed an anterior myometrial mass with dilated tortuous vessels in the lower uterine segment, indicative of scar ectopic pregnancy with arteriovenous malformation (AVM). An Magnetic resonance imaging (MRI) was performed to assess the extent of the lesion. The oncology profile was evaluated and cleared. Digital subtraction angiography confirmed the diagnosis. Bilateral uterine artery embolization successfully achieved complete devascularization, as confirmed on the post-intervention angiogram. The patient became symptom-free after that.
Interventional Radiology, specifically uterine artery embolization, serves as an effective treatment for arteriovenous malformation (AVM) and excessive vaginal bleeding. It presents a viable alternative to hysterectomy, particularly when preserving future fertility is a consideration.
Keywords
Scar ectopic pregnancy
Arteriovenous malformations
Uterine artery embolization
INTRODUCTION
Uterine arteriovenous malformations (AVMs) are characterized by abnormal and dysfunctional connections between the uterine arteries and veins.1 Acquired AVMs typically present in reproductive-age women, leading to menorrhagia as a result of uterine trauma, such as dilatation and curettage, cesarean delivery, or recurrent abortion. These acquired AVMs pose a serious threat to life, often necessitating blood transfusions.2,3
The management of acquired AVMs involves various approaches, and uterine artery embolization (UAE) has emerged as an effective and fertility-preserving intervention. UAE serves as an alternative to hysterectomy in women of childbearing age.4,5 This case report underscores the experience of a 26-year-old healthy woman who underwent bilateral super-selective uterine artery embolization to address severe uterine bleeding of unknown etiology during her pregnancy.
CASE REPORT
A 26-year-old woman, gravida 4, para 3, living 3 (G4P3L3), tested positive on a urine pregnancy test. She was referred to the Department of Radiodiagnosis due to excessive vaginal bleeding and lower abdominal pain. The clinical suspicion of ectopic pregnancy arose, given persistently elevated beta-HCG levels over 15 days. Initial reports from an external facility confirmed a non-endometrial pregnancy, and the patient had been undergoing methotrexate therapy.
Upon evaluation, transabdominal sonography (TAS) and transvaginal sonography (TVS) were conducted, revealing signs consistent with scar ectopic pregnancy and elements of a high-flow AVM. Subsequent confirmation of this diagnosis was obtained through magnetic resonance imaging (MRI).
At the time of presentation, the patient’s vital signs were within normal limits. However, her hemoglobin levels experienced a significant drop from 11.2 mg/dL upon admission to the Obstetrics and Gynaecology department to 7.9 mg/dL in just four days. Despite this, her coagulation profile remained normal. Doppler study exhibited a mosaic pattern of tangled vessels forming an AVM, characterized by a turbulent course, high velocity, and low resistance flow [Figure 1], consistent with AVM. A follow-up MRI was performed, affirming the ultrasound findings and assessing the extent of the condition, ultimately confirming the diagnosis of AVM following scar ectopic pregnancy [Figure 2].
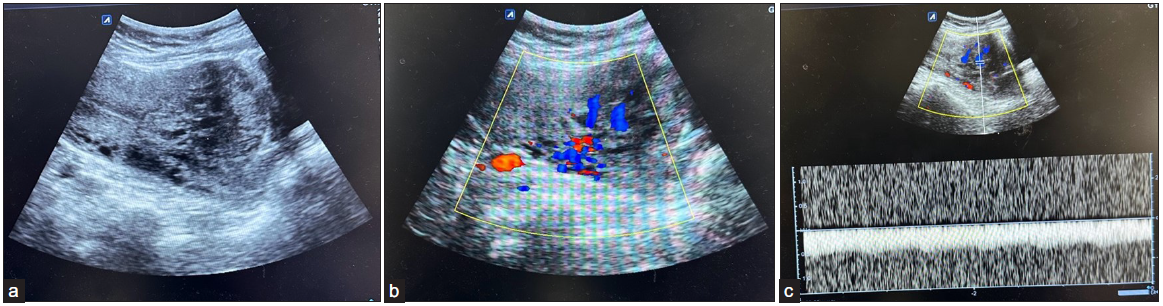
- (a) Ultrasound image showing 4.3 ´ 3.8 cm heterogeneous mass with multiple serpentine cystic spaces in anterior myometrium lower uterine segment close to previous cesarean scar site. (b) Color Doppler image shows high vascularity of the mentioned lesion, which shows high PSV and low RI waveform pattern, (c) suggesting the high-flow AVM component. PSV: Peak Systolic Velocity, RI: Resistive Index, AVM: Arterio-Venous Malformation.
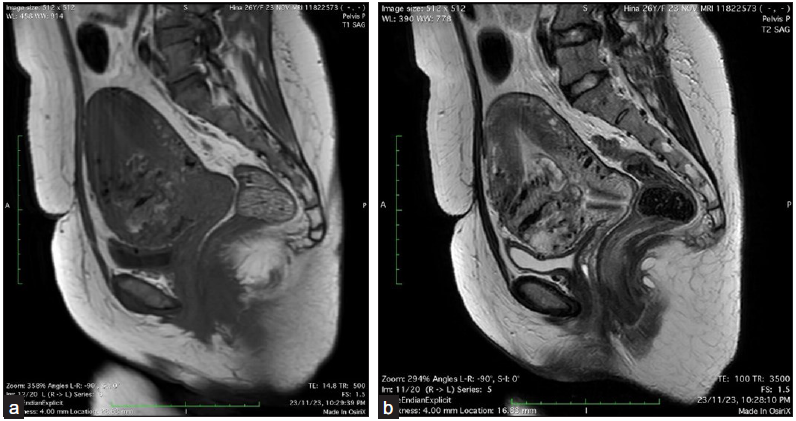
- (a) MRI pelvis shows an ill-defined T1 mixed and T2/short TI inversion recovery (STIR) heterogeneous hyperintense and, (b) mass lesion with multiple serpiginous T1 and T2 hypointense flow voids involving the lower uterine segment at previous cesarean scar site in anterior myometrium. STIR: short TI inversion recovery.
Considering the patient’s desire for future fertility and her reluctance to undergo major surgery, including a hysterectomy, UAE was planned. Digital subtraction angiography conducted via the right femoral artery approach revealed hypertrophied bilateral uterine arteries feeding the lesion [Figures 3a–3c]. The early enhancement of the nidus with a draining vein suggested a high-flow AVM with drainage into uterine veins. Bilateral UAE was performed using polyvinyl alcohol (PVA) particles (355–500 mm) and gel foam, achieving complete devascularization of the abnormal blush, as confirmed by post-procedure angiography [Figure 3d] and ultrasonography [Figure 3e]. The postoperative period was uneventful.
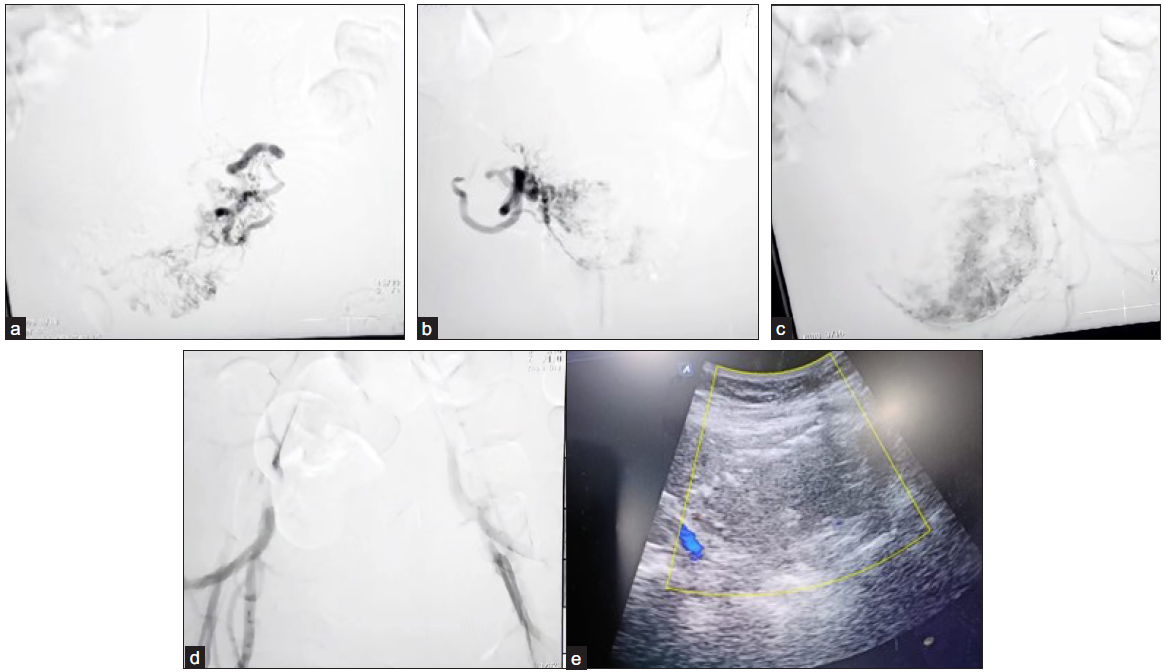
- (a-c) Angiography images show hypertrophied uterine arteries with parenchymal blush and draining veins. (d) Post embolization angiography reveals complete occlusion of the hypertrophied uterine vessels & disappearance of blush. (e) Immediate post-uterine artery embolisation (post-UAE) ultrasound demonstrates no significant flow on color Doppler within the lesion.
The patient was discharged the following day and remained under regular follow-up [Figure 4]. Her beta-HCG levels normalized after one week, and the abnormal vaginal bleeding was successfully halted.
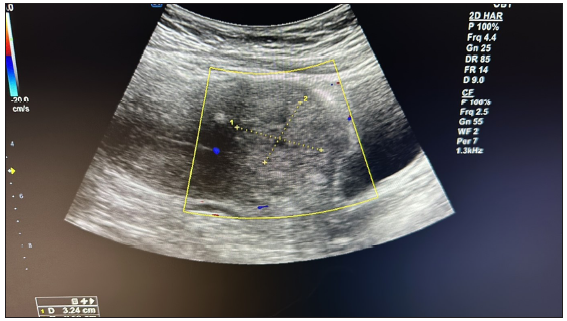
- Follow-up ultrasound after 30 days of intervention suggested a reduced size of the space-occupying lesion without any significant vascularity.
DISCUSSION
The true incidence of acquired arteriovenous malformation (AVM) remains uncertain due to its rarity. Existing literature reveals only a handful of cases where cesarean scar pregnancy is complicated by AVM.4 AVM can manifest with acute or chronic symptoms, with acute presentations often involving life-threatening hemorrhage, necessitating swift diagnosis and intervention. In contrast, our patient presented with chronic symptoms, specifically irregular vaginal bleeding. Although the pathogenesis of acquired AVM is not fully elucidated, it is theorized to result from arteriovenous fistulas developing within the placenta due to necrosis of chorionic villi or defective endometrium at the scar tissue, promoting abnormal angiogenesis.6
Diagnosing acquired AVM can be challenging, particularly in post-cesarean ectopic cases with clinical manifestations resembling retained products of conception (RPOC). Our case presented a diagnostic challenge, as persistent vaginal bleeding could be attributed to RPOC, AVM, or both. The diagnostic approach involves considering relevant clinical history alongside characteristic radiological findings. Color Doppler serves as an initial tool, displaying tortuous vascular structures with multidirectional flow indicative of AVM.7 However, AVM Doppler features may overlap with other causes of arteriovenous shunting, necessitating a high index of suspicion. Presently, CT/MRI angiography confirms the diagnosis, evaluates the lesion’s extent, delineates feeder vessels, and rules out extra-uterine involvement.8
Treatment options for AVM include expectant, medical, or surgical approaches tailored to symptomatology, lesion extent, and fertility desires. Fertility-sparing procedures are preferred for symptomatic young women. In our patient’s case, given her youth, desire for future fertility, and a large symptomatic lesion, bilateral UAE was performed. UAE has reported recurrences due to revascularization and potential complications, but our patient experienced cessation of flow, symptom resolution, and lesion regression without postoperative complications.
Surgical management involves lesion excision or hysterectomy. Our patient’s case allowed for precise planning of appropriate treatment, reducing morbidity and minimizing hospital visits. Notably, only a limited number of cases involving AVM complicating cesarean scar pregnancy have been reported in the literature (24 cases to date). Both cesarean scar pregnancy and AVM are potentially life-threatening conditions, and when coexisting, they pose the risk of catastrophic complications. UAE emerges as an effective mode of treatment for acquired AVM, highlighting the need for reporting more cases to establish references for early diagnosis and appropriate treatment.
The success rate of UAE varies, ranging from 61% for first-time transcatheter embolization (TCE) to 91% after the second embolization for persistent menorrhagia treatment.7 Regardless of advancements in therapeutic techniques and embolic agents, achieving fertility after successful embolization is contingent upon the vascularization of the placenta, identified as a primary cause of adverse pregnancy outcomes.8
Angiography is considered the “gold standard” for identifying feeding vessels in AVM.1 It is crucial to identify the dominant ovarian artery supply and the type of ovarian artery-to-uterine artery anastomosis for optimal outcomes, facilitating target embolization and preventing ovarian failure.
CONCLUSION
Early and precise diagnosis of arteriovenous malformation demands heightened clinical suspicion, particularly when risk factors such as uterine surgery are present. In instances like scar ectopic pregnancy or RPOC, diagnosis can be challenging, as seen in this case. Pelvic MRI plays a crucial role in confirming the diagnosis. Interventional radiologists play a vital role in the minimally invasive treatment of uterine artery embolization, proving to be an effective modality for managing complex cases involving morbid uterine AVM concurrent with cesarean scar pregnancy and coexisting RPOC. This approach offers a compelling alternative to hysterectomy, showcasing the importance of interventional radiology in the comprehensive management of such intricate conditions.
Acknowledgments
We extend our appreciation to the Departments of Radiodiagnosis and Obstetrics/Gynaecology at Gandhi Medical College, Bhopal, for the successful execution of Uterine Artery Embolization (UAE).
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Uterine arteriovenous malformations. Semin Ultrasound CT MR. 2021;42:37-45.
- [CrossRef] [PubMed] [Google Scholar]
- Acquired uterine arteriovenous malformation—a diagnostic dilemma. Ginekol Pol. 2018;89:227-8.
- [CrossRef] [PubMed] [Google Scholar]
- Uterine arteriovenous malformations induced after diagnostic curettage: A systematic review. Arch Gynecol Obstet. 2011;284:1137-51.
- [CrossRef] [PubMed] [Google Scholar]
- The influence of uterine artery embolisation on ovarian reserve, fertility, and pregnancy outcomes—a review of literature. Prz Menopauzalny. 2016;15:205-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Menopause and menopausal symptoms after ovarian artery embolization: A comparison with uterine artery embolization controls. J Vasc Interv Radiol. 2011;22:710-715.e1.
- [CrossRef] [PubMed] [Google Scholar]
- Conservative treatment of uterine arteriovenous fistula. Acta Obstet Gynecol Scand. 1982;61:85-7.
- [CrossRef] [PubMed] [Google Scholar]
- A systematic review of acquired uterine arteriovenous malformations: Pathophysiology, diagnosis, and transcatheter treatment. AJP Rep. 2016;6:e6-e14.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Uterine vascular lesions. Rev Obstet Gynecol. 2013;6:69-79.
- [PubMed] [PubMed Central] [Google Scholar]







