Translate this page into:
Transient elastography for non-invasive assessment of liver fibrosis
* Corresponding author: Dr. Piyush Manoria, DTCD, MD, DM (Gastroenterology), FASGE, Chief Gastroenterologist & Hepatologist, Department of Gastroenterology, Manoria Hospital, Bhopal, Madhya Pradesh, India. manoria_piyush@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Manoria P. Transient elastography for non-invasive assessment of liver fibrosis. Future Health. 2024;2:206-10. doi: 10.25259/FH_73_2024
Abstract
Accurate estimation of liver fibrosis is important for determining the stage of liver disease, for making therapeutic decisions, and for assessing the prognosis of patients. Though liver biopsy is the traditional gold standard for assessing liver fibrosis, various non-invasive methods that can substitute it are now available . Transient elastography is the most reliable and validated non-invasive method for measuring liver fibrosis in routine clinical practice. It can be performed in an outpatient department (OPD) with immediate results and excellent reproducibility. It has been evolved in the past decade to become an essential tool in the management of chronic liver disease.
Keywords
Elastography
Fibrosis
Liver
INTRODUCTION
Chronic liver disease is a global health problem. Liver fibrosis, which leads to liver cirrhosis, portal hypertension, liver failure, and hepatocellular carcinoma is the end result of any chronic liver disease. Early and accurate estimation of liver fibrosis is essential for preventing its complications and for prognostication. Though liver biopsy is the traditional gold standard for estimation of liver fibrosis, its use has decreased over the last decade due to its invasive nature, risk of complications, and sampling error. Various non-invasive methods have been developed for the estimation of liver fibrosis : 1) Transient Elastography (TE), 2) Shear wave elastography (SWE), 3) Magnetic resonance elastography (MRE), and 4) Serum biomarkers. Out of all these, TE is the most validated and reliable method for the diagnosis of liver fibrosis and is currently approved for use in Asia, Europe, and the United States.1
PRINCIPLE OF TE
The basic principle of TE is that the propagation velocity of a wave through a homogenous tissue is proportional to its elasticity, which correlates to the amount of fibrosis in the liver.2 It consists of an ultrasound transducer probe of 5 MHzmounted on the vibrator axis, which produces vibrations of mild amplitude and low frequency of 50 Hz. These vibrations produce elastic shear waves which propagate through the liver. Ultrasound reflection follows these waves and measures their velocity which is directly related to tissue stiffness [Figure 1].3 More the fibrosis in the liver, the faster the wave propagates and more will be the liver stiffness measurement (LSM) which is expressed in kilopascals (kPa) (Normal range:2.5-75 kPa).
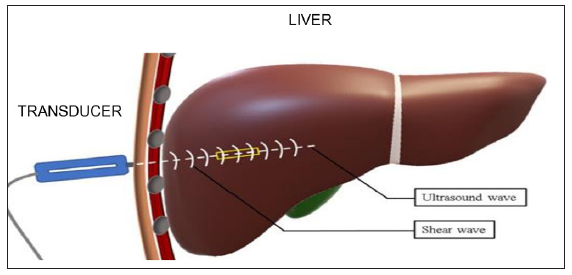
- Principles of transient elastography.
TE measurement is well tolerated in most patients. It is measured by a hand-held probe, which is placed in the right lobe of the liver through the 9-11th intercostal space in the right axillary line with the patient lying in the dorsal decubitus position with the right arm in maximum abduction.3 The operator locates the probe in a liver portion free of vascular structures and gallbladder by a time motion ultrasound image and presses the probe button to commence the measurement. About 10 valid measurements should be performed and an average value of these measurements is considered to represent liver elasticity. TE measurement is considered valid if these three criteria are fulfilled: 1) At least 10 valid shots of measurement, 2) Success rate (i.e., the ratio of valid shots to the total number of shots) higher than 60%, and 3) Interquartile range (IQR) which reflects the variability of validated measurements should not exceed 30%.4
Currently, there are two instruments available for measuring LSM. First is the Fibroscan (Echosens, Paris France), which was introduced in 2003 and was approved by US FDA in 2013. It has two types of probes for different skin liver capsule distances: M probe for 25–65mm distance and XL probe used for obese persons for 35–75 mm distance. The second instrument is the Fibrotouch (Hisky Wuxi China), which has been available since 2013 and has been US FDA approved since 2018. It has a single probe that can detect the thickness of subcutaneous fat and adjust the emission of appropriate ultrasonic frequency. LSM of both these instruments are comparable with each other.5
TE is an OPD procedure with a short procedure time, which gives immediate results and can be performed by a nurse or technician.
NORMAL VALUES OF TE
Mean liver stiffness in a healthy population is 5.5 + 1.6 kPa, with values higher in men than in women (5.8 + 1.5 vs 5.2 + 1.6 kPa, respectively; p=0.0002).6
CONFOUNDING FACTORS IN MEASUREMENT OF TE
Food intake: TE should be ideally done after three hours of fasting, as meals can overestimate the degree of fibrosis due to increased portal inflow.
Acute hepatitis: Its measurement is unreliable in acute elevation of transaminases as LSM values increases by 1.3 to 3 folds in alanine transaminases (ALT) flares, which can lead to a false diagnosis of cirrhosis.7 So, it is advisable to avoid TE in acute hepatitis or to repeat its measurement after recovery from acute liver injury. Caution should be applied in its measurement when ALT levels are above 100 IU/L.
Right heart failure: TE is not suitable for measurement of liver fibrosis in right heart failure with liver congestion and tricuspid regurgitation as it will lead to an overestimation of LSM value.
Biliary obstruction: Extrahepatic cholestasis will increase LSM values and will lead to an overestimation of liver fibrosis. TE values declined significantly after biliary drainage. TE should be avoided if bilirubin is > 10 mg/dL and should be repeated after biliary drainage when bilirubin levels come to normal.
Obesity: Standard M probe in the Fibroscan has a higher failure rate in obese patients with high BMI (>30kg/m2) and increased waist circumference due to interference of shear waves and ultrasound waves through liver parenchyma by thick subcutaneous fat. So, if the skin-capsule distance is > 2.6 cm, an XL probe with lower ultrasound frequency, greater transducer focal length and measurement depth of 35-75mm should be used The M probe has a measurement depth of only 25–65mm.
Operator experience: TE is an operator-independent procedure with a high interobserver agreement up to 98%. It is suggested that a minimum experience of 50 TE measurement is essential for the operator to perform it independently, and its reliability is increased with more than 500 previous measurements.8
Other factors: TE measurement is difficult in patients with narrow intercostal space due to a poor window. In ascites, there is a high rate of unsuccessful LSM due to the interruption of shear waves by it. It is contraindicated in pregnancy and patients with cardiac pacemakers.
CLINICAL APPLICATION OF TE
Non-Alcoholic Fatty Liver Disease (NAFLD):
NAFLD is a spectrum of diseases ranging from simple steatosis, which is a benign disease, to non-alcoholic steatohepatitis (NASH), an aggressive disease that can progress to cirrhosis and hepatocellular cirrhosis (HCC). So, accurate staging of fibrosis is very important in the management of NAFLD. TE is very useful to estimate the severity of liver fibrosis in these patients. The cut-off values for F2, F3, and F4 fibrosis reported in various studies are 6.6-7.8, 7.1-10.4, and 10.3-22.3 kPa, respectively.9 In a recent large meta-analysis, it was found that TE has excellent accuracy in diagnosing F4 fibrosis (92% sensitivity, 92% specificity) and F3-4 fibrosis (85% sensitivity, 82% specificity) and moderate accuracy for F2 or higher fibrosis (79% sensitivity, 75% specificity).10
TE is also useful to screen the high-risk population for liver fibrosis such as people with Type 2 diabetes and obesity.
It is useful for selecting patients for pharmacological treatment and clinical trials. It can also be very useful to follow these patients to see the efficacy of drugs on liver stiffness.
Along with LSM, it can also detect the amount of hepatic steatosis by measuring the controlled attenuation parameter (CAP) in dB/m, which estimates the ultrasound attenuation at the central frequency of TE. It can detect more than 5% of hepatic steatosis compared to conventional ultrasound, which can only detect more than 30% of steatosis.
Chronic hepatitis B (CHB):
It is important to distinguish active disease from inactive disease in CHB, as the former will progress to advanced fibrosis and cirrhosis. There is a subset of patients who have normal transaminases but a high degree of fibrosis. TE is useful in such a subset of patients and can find those having significant fibrosis as they are candidates for antiviral therapy. In CHB, an LSM of <6 excludes significant liver disease, >8 indicates significant fibrosis (F>2), and > 11 suggests cirrhosis.11
TE can also be used to monitor CHB patients on antiviral therapy, as fibrosis regression can be achieved by suppressing the replication of HBV.
Chronic hepatitis C (CHC): TE was first developed and validated in patients with CHC. TE values significantly correlate with histological fibrosis stages and have high diagnostic accuracy. TE cut-off value of 12.5 kPa is used to detect cirrhosis in CHC.12 With the paradigm shift in the management of CHC, the role of non-invasive markers for the detection of fibrosis has diminished. All CHC patients should be offered treatment irrespective of the severity of fibrosis, as a cure is possible. TE can be used to monitor CHC patients on treatment as antivirals can regress the fibrosis and reduce the risk of cirrhosis.
Predicting liver-related complications: TE not only allows early identification of patients with advanced fibrosis but can also predict liver related complications in compensated advanced chronic liver diseases such as variceal bleeding, hepatocellular carcinoma, and liver-related death. Upper GI endoscopy screening for varices has been recommended for cirrhotic patients, but it is inconvenient and invasive. The Baveno VI consensus proposes that patients with platelets > 150000 and LSMM <20 kPa exhibit a very low risk of having high risk varices and they can safely avoid screening endoscopy.13 Also, studies have found a positive correlation with development of hepatocellular carcinoma and the risk of death with a higher degree of fibrosis.
Alcoholic liver disease: TE can be used to rule out liver cirrhosis in alcoholic liver disease using a cut-off value of 12.5 kPa, and its performance is better than other biochemical non-invasive markers.
Cholestatic liver disease: In primary biliary cirrhosis and primary sclerosing cholangitis, TE is a reliable non-invasive marker for assessing fibrosis stage superior to other available biochemical non-invasive markers.
Non-cirrhotic portal hypertension (NCPH): TE is used to exclude cirrhosis in patients with NCPF who present with clinical features of cirrhosis. LSM is much lower in NCPF as compared to cirrhotics in the range of 8–9 kPa.
Methotrexate (MTX) related liver toxicity: It’s a reliable non-invasive tool for monitoring MTX-related liver toxicity and can avoid routine liver biopsy.
TE is the most accurate non-invasive test for diagnosis of cirrhosis with a high negative predictive value to exclude liver cirrhosis.
COMPARISION OF TE WITH OTHER NON-INVAISVE MARKERS OF FIBROSIS
SWE: SWE measures the speed of propagating shear waves, travelling perpendicular to the axis of an applied force generated by ultrasound-induced acoustic radiation. This shear wave is calculated in m/s and is converted to elasticity using Young’s module into kPa. It arrived in the market in 2009, and currently all ultrasound manufacturers have developed their own liver stiffness quantification modality. SWE is of two types:
Point SWE (pSWE) or acoustic radiation force impulse imaging (ARFI):(Available with Siemens Acuson S2000/S3000 and Philips EPIQ 7/EPIQ 5) in which the shear wave is calculated in a tiny portion of tissue of 0.5 to 1cc.
-
2D SWE:(Available with Supersonic imagine GE logic E9/E10 and Canon Aplio 500) where the shear wave is calculated in a larger field of view of 14–20 cc.
Advantages of SWE over TE are:
It has a slightly higher success rate than TE especially in patients having ascites and obesity.
It allows the handleravoid placing the region of interest over potential masses, gall bladder, bile ducts, and blood vessels.
Ultrasound examination can be done in the same setting.
Disadvantages of SWE over TE are:
It’s operator dependent and needs to be performed by an experienced sinologist.
It is not widely available.
It is not fully validated and the grade of recommendation is lower than TE.14
-
MRE: It uses the modified phase contrast technique to visualize the propagation characteristics of acoustic shear waves generated by an acoustic driver placed over the liver.
Advantage of MRE over TE:
It can assess the whole liver.
It does not depend on the operating person.
It can be performed in fatty individuals and with free fluid in the abdomen.
Disadvantage of MRE over TE:
It is expensive.
It is not available easily.
It has a long examination time.
It cannot be done when the liver has iron overload.
-
Serum markers: TE and serum markers are comparable to each other for the diagnosis of fibrosis in the liver, but TE has better accuracy for the diagnosis of cirrhosis.
Advantage of serum markers over TE:
It is fluently available.
It is affordable.
It can be done without any special instruments or specific training.
Disadvantages of serum markers over TE:
It is an indirect marker of liver fibrosis.
It measures liver fibrosis indirectly.
The results can be confounded by biochemical abnormalities.
Some tests are personal and expensive.
CONCLUSION
TE has now become an essential and established tool in the management of liver diseases. It has become an excellent, non-invasive, rapid, accurate, easy to perform, and validated tool for the quantitative assessment of liver fibrosis. It is the most accurate, non-invasive method for diagnosing liver cirrhosis. It is a highly reproducible technique for assessing liver fibrosis in patients with CLD and to predict complications and prognosis of cirrhosis.
Author contributions
PM: Drafted, edited and made the final proofing of the manuscript.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent is not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
REFERENCES
- Clinical applications, limitations and future role of transient elastography in the management of liver disease. World J Gastrointest Pharmacol Ther. 2016;7:91-106.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Elastic modulus measurements of human liver and correlation with pathology. Ultrasound Med Biol. 2002;28:467-74.
- [CrossRef] [PubMed] [Google Scholar]
- Liver ultrasound elastography: Review of techniques and clinical applications. R I Med J (2013). 2020;103:26-9.
- [PubMed] [Google Scholar]
- Clinical applications of transient elastography. Clin Mol Hepatol. 2012;18:163-73.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Comparison of FibroTouch and FibroScan for staging fibrosis in chronic liver disease: Single-center prospective study. Dig Liver Dis. 2019;51:1323-1329.
- [CrossRef] [PubMed] [Google Scholar]
- Liver stiffness values in apparently healthy subjects: Influence of gender and metabolic syndrome. J Hepatol. 2008;48:606-13.
- [CrossRef] [PubMed] [Google Scholar]
- Transient elastography is unreliable for detection of cirrhosis in patients with acute liver damage. Hepatology. 2008;47:592-5.
- [CrossRef] [PubMed] [Google Scholar]
- The feasibility and reliability of transient elastography using Fibroscan®: A practice audit of 2335 examinations. Can J Gastroenterol Hepatol. 2014;28:143-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Measurement of liver stiffness as a non-invasive method for diagnosis of non-alcoholic fatty liver disease. Hepatol Res. 2015;45:142-51.
- [CrossRef] [PubMed] [Google Scholar]
- Systematic review with meta-analysis: Non-invasive assessment of non-alcoholic fatty liver disease--the role of transient elastography and plasma cytokeratin-18 fragments. Aliment Pharmacol Ther. 2014;39:254-69.
- [CrossRef] [PubMed] [Google Scholar]
- Asian-Pacific clinical practice guidelines on the management of hepatitis B: A 2015 update. Hepatol Int. 2016;10:1-98.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- American gastroenterological association institute guideline on the role of elastography in the evaluation of liver fibrosis. Gastroenterology. 2017;152:1536-1543.
- [CrossRef] [PubMed] [Google Scholar]
- Validating and expanding the Baveno VI criteria for esophageal varices in patients with advanced liver disease: A multicenter study. Ann Gastroenterol. 2020;33:87-94.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Non-invasive tests for evaluation of liver disease severity and prognosis. J Hepatol. 2015;63:237-64.
- [CrossRef] [PubMed] [Google Scholar]







