Translate this page into:
The prevailing social stigma around disorders of sexual development in developing countries
Corresponding author: Prof. Amit Nandan Dhar Dwivedi, Institute of Medical Sciences, Banaras Hindu University, Varanasi, India. amitnandan21@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Dwivedi AND, Yadav N, Yadav V. The prevailing social stigma around disorders of sexual development in developing countries. Future Health. 2024;2:90–93. doi: 10.25259/FH_3_2024.
Abstract
Disorders of sexual development (DSD), apart from medical disease, is a psychosocial stigma to not only the patient but also their whole family. We present the case of a 24-year-old 46XX, raised as male, with ambiguous genitalia and cyclical hematuria with normal female internal genitalia and secondary sexual characteristics. This case underscores the influence of social stigma and the psychosocial vulnerability associated with DSD on individuals’ lives in developing countries.
Keywords
socioeconomic
androgen exposure
gender assignment
virilization
gonadal dysgenesis
INTRODUCTION
Disorders of sexual development (DSD) were defined in the Chicago Consensus, 2006 as congenital conditions in which the development of chromosomal, gonadal, and anatomical sex is atypical, estimated to affect 1/4,500–5,500 births.1 DSD, because of excessive androgen exposure, can be detected at birth as abnormal genitalia or later in life, usually at puberty because of virilization. The clinical picture can vary from virilized females with enlarged phallus/clitoris, which can be confused with male genitalia and hence leading to rearing the child as male. The main aim of treatment in such cases is gender assignment, which, if done earlier, can prevent mental agony in patients. If not done in time, in societies where males enjoy privileged financial and social status, there might be heightened pressure to raise children as males. However, to determine the future fertility of the patient, imaging plays a crucial role in identifying mullerian structure development.
CASE REPORT
A 24-year-old, raised as male since birth, visited the Department of Urology with complaints of small male genitalia. Physical examination revealed micropenis, penoscrotal meatus, and nonpalpable gonads. The patient was referred to the Department of Endocrinology and Department of Radiodiagnosis and Imaging for further workup.
The patient gave a history of cyclical hematuria for the last 18 years. On physical examination, there was no feature of hirsutism. Examination of breast and genitalia was done after obtaining the patient’s consent. Breasts were developed (Tanner stage 4) [Figure 1a]. Examination of genitalia revealed a phallus with a length of 3 cm, the labioscrotal forum was incomplete, and the single opening was noted [Figure 1b].

- (a) Shows a fully developed breast (Tanner stage 4). (b) shows a phallus length of 3 cm, labioscrotal forum was incomplete, and single genito-urinary opening.
On ultrasonography [Figure 2], an anteverted uterus was seen, normal in size, measuring approximately 7.3 × 3.0 (longitudinal × anteroposterior), with normal echotexture. Endometrial thickness measured 5.2 mm. Bilateral ovaries were normal in location. An endometriotic cyst was noted in the left ovary. The testicular structure was not visualized. Ultrasound of the breast revealed normal proliferation of the fibroglandular tissue. Further, to rule out the possibility of the presence of ovotestis, an magnetic resonance imaging (MRI) of the whole abdomen [Figure 3] was done, which revealed similar findings as ultrasonography. Testis was not found.

- Anteverted symmetric uterus with normal outer contour, normal size, echotexture, and endometrial thickness.
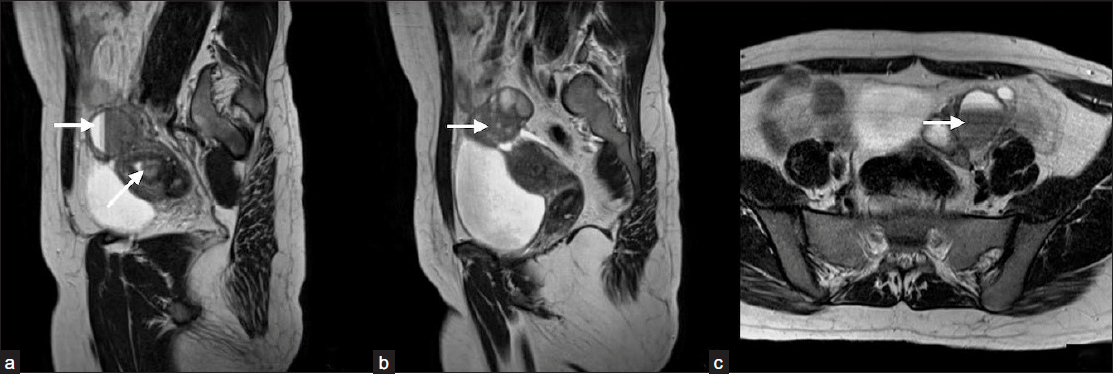
- (a and b) Show a uterus with normal size, shape, and position with endometrial collection (arrow in 3a). (b and c) show bilateral endometriosis cysts (arrows in 3a, 3b, 3c).
Karyotyping was performed and showed a 46XX karyotype.
A hormonal evaluation of the patient was done, which came out to be normal.
Diagnosis of 46XX DSD was made, and probable causes include exposure to exogenous androgens or maternal androgen-secreting tumor.
The patient was counseled for clitoroplasty; however, the patient did not agree, and the risk of loss of complete fertility after the surgery was explained.
DISCUSSION
DSDs were defined in the Chicago Consensus, 2006 as congenital conditions in which the development of chromosomal, gonadal, and anatomical sex is atypical, estimated to affect 1/4,500–5,500 births.1
DSD in a biological female (46 XX) can be classified as:
-
1.
Disorder of gonadal differentiation—present with palpable gonads, pubertal gynecomastia, and the presence of mullerian structures. This includes testicular DSD, ovotesticular DSD, and primary ovarian insufficiency.
-
2.
Disorder with an excessive amount of androgen—present as impalpable gonads and virilization (clitoromegaly). This includes excessive androgen exposure in the fetus as congenital adrenal hyperplasia, virilizing ovarian or adrenal tumor, and placental or maternal causes.
-
3.
Others include Mayer–Rokitansky–Küster–Hauser (MRKH) syndrome, cloacal exstrophy, vaginal atresia, labial fusion, etc.
In our patient with cyclical hematuria, apart from DSD, other differentials of such presentation on imaging is congenital vesicovaginal fistula with transverse vaginal septum. Another differential could be an iatrogenic uretero-vesico-vaginal fistula, which could be formed due to iatrogenic injury from any surgical repair done during childhood. However, in our patient, as there was no history of previous surgical/medical intervention and because of the presence of ambiguous genitalia, a diagnosis of DSD was made. Among DSD, differentials of ambiguous genitalia with mullerian structures include gonadal dysgenesis and androgen-secreting tumor. However, because of failure to visualize testicular structures and normal hormonal analysis, other differentials were ruled out.
Because of excessive androgen exposure, DSD can be detected at birth as abnormal genitalia or later in life, usually at puberty because of virilization. The clinical picture can vary from virilized females with enlarged phallus/clitoris, which can be confused with male genitalia and hence leading to rearing the child as male. Associated symmetric but variable degrees of labial fusion can be seen with variable urethral and vaginal orifice as common urogenital sinus to separate openings. During puberty, hyperpigmentation of the perineum, axilla, and areola can be noted with pubic hairs and breast development. Because of the presence of functional mullerian structures, the female remains fertile. Because of this, imaging is critical to aid in diagnosis to identify mullerian structures and their development.
The main aim of treatment in such cases is gender assignment, which if done earlier can prevent mental agony in patients. The main aim of gender assignment is to preserve fertility and help patients to lead a somewhat better life.
The gender assignment to be done is decided by various factors:2-
-
When is the surgery performed?—if done earlier in life, preserving fertility can be the aim of assigning the gender.
-
Psychosocial outcome—considering the fact, till surgery, what was the gender assigned to the patient from birth.
-
Need for other lifelong treatment, for example, hormonal replacement therapy.
As in our case, to preserve fertility, the patient was advised to undergo female gender assignment. However, as the individual was reared as male, the family opted for male gender assignment.
Regardless of socioeconomic or educational background, the birth of a child with DSD is still perceived as a major medical and social problem by most parents. Ideally, individuals with DSD should receive a diagnosis and appropriate treatment during their infancy. However, in developing countries like India, though the trends are changing, due to limited medical resources and various social constraints, a significant number of patients do not receive timely diagnosis and treatment.3
One primary concern is that due to social infamy and limitations in infrastructure, numerous cases of DSD do not seek clinical care until they reach adolescence or even adulthood.
Cultural contexts significantly influence the decisions regarding gender assignment or “sex of rearing,” particularly with the influence of religious and traditional beliefs on parental choices. In societies where males enjoy privileged financial and social status, there might be heightened pressure to raise children as males.4
Another critical issue is the lack of awareness, which extends beyond the general population to include hospital staff and the medical community. Often, parents have been advised by doctors not to be overly concerned about their child’s genitalia at the moment, and to seek assistance later if the child does not undergo sexual development during puberty. Numerous DSD patients experienced ridicule from hospital staff, which deterred them from seeking medical care. Furthermore, frequent genital examinations have been recognized as a contributor to diminished quality of life and discontentment.5
This case underscores the influence of social stigma and the psychosocial vulnerability associated with DSD on individuals’ lives in developing countries. The fear of humiliation hindered the patient from discussing the condition even with their parents, resulting in a delayed diagnosis. The patient discontinued their education because they were afraid of being ridiculed. Despite being aware of the possibility of having a successful pregnancy in the future, the individual decided to identify as male. Their choice was motivated by the fear that nobody would be willing to marry a woman who had lived as a man, which would subject their entire family to ridicule in society. They also expressed that remaining unmarried as a male would be a more manageable situation for their social survival than staying unmarried as a female.
If the patient had received an earlier diagnosis and appropriate treatment, it could have prevented the psychological trauma endured by both the patient and their family throughout their life. Furthermore, the extensive surgical procedures the patient is now facing could have been avoided and they could have lived a simpler life. Living with DSD is hard and even harder for the patients living in a society that neither understands nor supports patients with DSD. The patient’s psychological distress is difficult to comprehend.
Clear communication, precise diagnosis, and comprehensive multidisciplinary care are essential to alleviate psychological distress for both the patient and their family. Social intervention is required to endorse social acceptance for individuals with DSD and their families. Equally significant is the need for comprehensive training and education of hospital staff. Both the medical and paramedical personnel comprehend the sensitivity surrounding this subject. Establishing efficient referral pathways to tertiary centers, when feasible, would be advantageous. Early surgical intervention and gender reassignment were encouraged with a view to improving parental psychological distress. Due to the heterogeneity of the disorders, care must be individualized.6 Finally, utilizing validated quality-of-life measures and systematic, regular screening of psychosocial outcomes will help identify targeted areas to improve psychological status.7 Further research and education will be necessary to improve standards of care in the developed, and particularly the developing world.
CONCLUSION
Disorders of sexual development, apart from medical disease, is a psychosocial stigma to not only the patient but his/her whole family. Clear communication, precise diagnosis, and comprehensive multidisciplinary care are essential to alleviate psychological distress for both the patient and their family. Social intervention is required to endorse social acceptance for individuals with DSD and their families. Imaging is critical to aid in diagnosis to identify mullerian structures and there development.
Data availability
The data that support the findings of this study are available on request from the corresponding author. The data is not publicly available due to the information that could compromise the privacy of the patient.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The author certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Global DSD Update Consortium. Global disorders of sex development update since 2006: perceptions, approach and care. Hormone research in paediatrics. 2016;85:58-180.
- [CrossRef] [PubMed] [Google Scholar]
- How common is intersex? A response to Anne Fausto-Sterling. J Sex Res. 2002;39:174-8.
- [CrossRef] [PubMed] [Google Scholar]
- Management guidelines for disorders/different sex development (DSD) Anales de Pediatría (English Edition). 2018;89:315-e1.
- [PubMed] [Google Scholar]
- Clinical, etiological and laboratory profile of children with disorders of sexual development (DSD)-experience from a tertiary pediatric endocrine unit in Western India. Indian J Endocrinol Metab. 2021;25:48-53. IJEM_520_20. Epub 2021 Jul 21
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Barriers in access to healthcare services for individuals with disorders of sex differentiation in Bangladesh: an analysis of regional representative cross-sectional data. BMC Public Health. 2020;20:1261.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The psychosocial impact of disorders of sexual development. Journal of Sexual Medicine and Reproductive Health. 2019;2:4.
- [Google Scholar]
- Quality of health care in adolescents and adults with disorders/differences of sex development (DSD) in six European countries (dsd-LIFE) BMC Health Serv Res. 2018;18:1-12.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- DSD‐TRN Psychosocial Workgroup, the DSD‐TRN Advocacy Advisory Network, and Accord Alliance. Interdisciplinary care in disorders/differences of sex development (DSD): The psychosocial component of the DSD—Translational research network. In Am J Med Genet C Semin Med Genet. 2017;175:279-92.
- [Google Scholar]