Translate this page into:
Omphalocele with umbilical cord cyst and mesomelia: A case report
Corresponding author: Dr. Ashok Jangda, Department of Radiodiagnosis, MGMMC & MYH, Indore, MP, India. jangdaashok@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Jangda A. Omphalocele with umbilical cord cyst and mesomelia: A case report. Future Health. 2024;2:78–81. doi: 10.25259/FH_13_2024
Abstract
Omphalocele is a rare congenital abdominal wall defect with a reported prevalence of 3.38 per 10,000 pregnancies. It is associated commonly with chromosomal abnormalities (10%–30%) and additional structural abnormalities (55%–58%). Trisomy 13 and 18 are most commonly associated with aneuploidies, which are also associated with umbilical cord cysts and mesomelia.
Keywords
Omphalocele
umbilical cord cyst
mesomelia
INTRODUCTION
Omphalocele refers to herniation of the intestine and other abdominal organs into the base of the umbilical cord through an abdominal wall defect.1–3 Most cases of omphalocele are readily detected at the time of the second trimester scan as protrusion of abdominal contents into the base of the umbilical cord contained within a sac.4
Umbilical cord cysts can be seen throughout pregnancy, occurring most frequently in the segment closest to the fetus.5 Umbilical cord cysts are associated with both structural and chromosomal defects like Trisomies 13 and 18 and genitourinary and gastrointestinal anomalies, so a detailed structural survey is required whenever a cyst is encountered.6
Mesomelia refers to the shortening of the middle segment (radius/ulna, tibia/fibula) of the fetus. This is in contrast to rhizomelic dwarfism, in which the proximal segments of limbs are shortened, such as in achondroplasia and acromelia, in which there is shortening of hands and/or feet.7
CASE REPORT
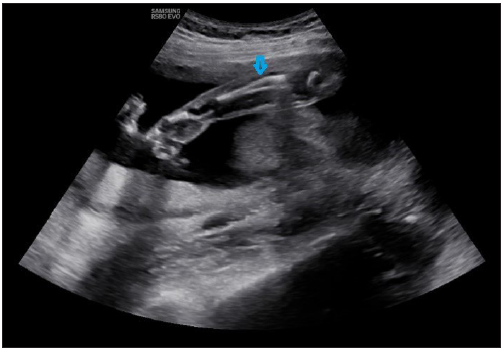
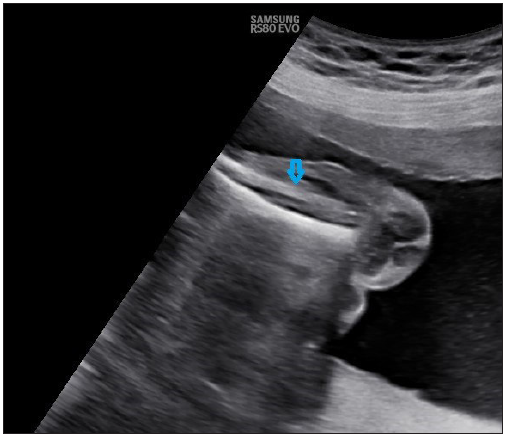
A 26-year-old primigravida was referred to the hospital for second trimester anomaly scan at 23 weeks gestational age. An obstetric scan was done, which showed the fetus in cephalic presentation. The placenta was anterior, well away from the internal os. Amniotic fluid was adequate. Routine fetal biometric parameters, namely, biparietal diameter, head circumference, abdominal circumference, and femur length were recorded, which were found to be appropriate for gestational age. No significant abnormality was noted in the fetal central nervous system and cardiothoracic system. The scan revealed a ∼3.9 cm sized midline anterior abdominal wall defect in the fetus in the umbilical region with herniation of fetal bowel loops, which was also covered by a membrane suggesting omphalocele [Figure 1]. A well-defined unilocular cystic lesion measuring ∼1.9 × 1.1 cm was seen within the umbilical cord, suggestive of umbilical cord cyst [Figure 2].5 The bones of the middle segment of both upper and lower limbs, i.e., radius, ulna, tibia, and fibula, appeared short for gestational age, suggesting mesomelia [Figures 3 and 4].
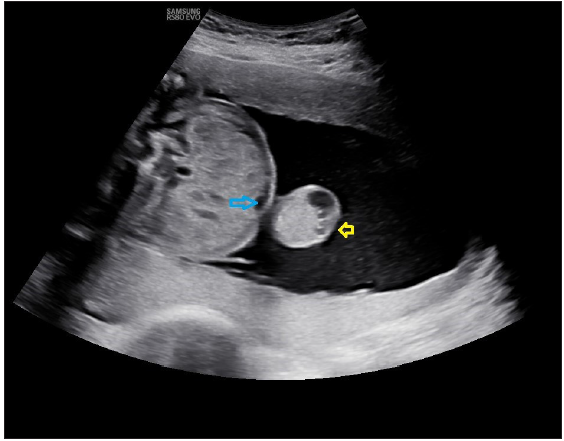
- Midline anterior abdominal wall defect in fetus in umbilical region with herniation of fetal bowel loops, covered by a membrane, suggesting omphalocele. Blue arrow showing a defect in the umbilical region. Yellow arrow showing hernial sac with bowel loops as content.
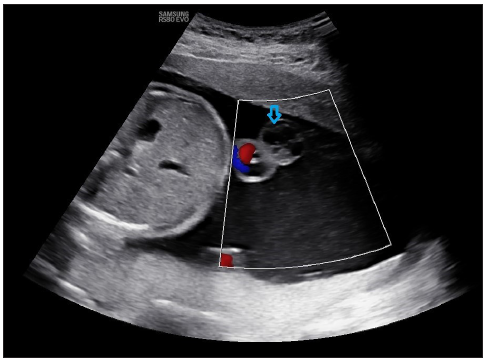
- Cystic lesion (blue arrow) is seen arising from the umbilical cord, suggesting an umbilical cord cyst, which does not show vascularity on color doppler imaging.
- (blue arrow) Radius and ulna, which were short for gestational age (19 weeks ±two days) as measured by Merz and Jeanty formula suggesting Mesomelia.
- (blue arrow) Tibia and fibula, which were short for gestational age (19 weeks ±two days) as measured by Merz and Jeanty formula suggesting Mesomelia.
No other significant abnormalities were detected in the fetus.
The overall Estimated Gestational Age (EGA) by USG was 23 weeks two days ± two weeks, by using the biparietal diameter, head circumference, abdominal circumference, and femur length [Table 1]. However, the average EGA was 19 weeks two days ± two weeks according to the measurements of radius, ulna, tibia, and fibula length. The effective fetal weight was 603 grams ± 10%.
| Parameter | Author (Formula used) | Value | Gestational age |
|---|---|---|---|
| Biparietal diameter | Hadlock | 5.70 cm | 23 weeks 3 days |
| Head circumference | Hadlock | 21.14 cm | 23 weeks 2 days |
| Abdominal circumference | Hadlock | 18.67 cm | 23 weeks 3 days |
| Ulna length | Jeanty | 2.54 cm | 19 weeks 1 days |
| Tibia length | Jeanty | 2.65 cm | 19 weeks 3 days |
| Fibula length | Jeanty | 2.67 cm | 19 weeks 2 days |
| Radius length | Merz | 2.39 cm | 19 weeks 3 days |
| Femur length | Hadlock | 4.11 cm | 23 weeks 2 days |
The final diagnosis was an omphalocele with the umbilical cord cyst and mesomelia.
It is noteworthy that the ideal time for a second-trimester anomaly scan is 18–22 weeks, so early intervention is possible if needed. A nuchal translucency scan (11–13 weeks) is also able to diagnose an abdominal wall defect like omphalocele. But in our case, the patient didn’t undergo any obstetrics scan previously and presented to our hospital at 23 weeks, causing a delay in the diagnosis. Karyotyping is recommended as the next step, which could not be done in this case due to patient’s refusal.
DISCUSSION
Physiological midgut herniation is usually visible on ultrasound from 9 to 11 weeks and resolves by 12 weeks of gestation.
The persistence of the midgut herniation beyond 12 weeks or the presence of content other than intestine (e.g., liver) in the hernial sac should raise the suspicion of an abdominal wall defect (i.e., omphalocele) [Figure 1]. The spectrum of severity ranges from a small hernia to a large defect, resulting in evisceration of all abdominal organs.1–3
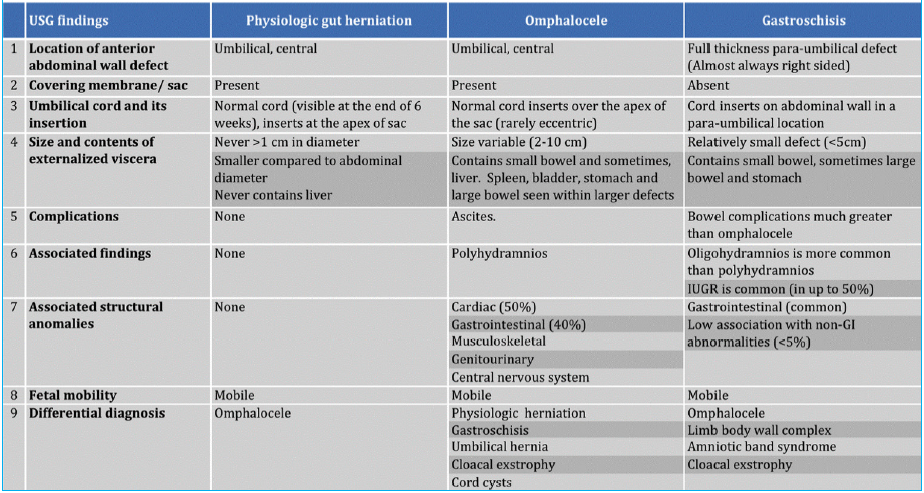
Gastroschisis is another type of anterior abdominal wall defect that needs to be considered as a differential diagnosis. As shown elaboratively in Table 2, the differences between physiological gut herniation, omphalocele, and gastroschisis..
Syndromes associated with omphalocele include the following:
-
Trisomy 13 (Patau syndrome)
-
Trisomy 18 (Edwards syndrome)
-
Trisomy 21 (Down syndrome)
-
Pentalogy of Cantrell
-
Limb body wall complex
-
Shprintzen–Goldberg syndrome
-
Charge syndrome
-
Cloacal exstrophy (OEIS)
-
Carpenter syndrome
-
Marshall–Smith syndrome
-
Meckel–Gruber syndrome
The overall prognosis of patients with omphalocele predominantly depends on associated chromosomal or structural anomalies.
Umbilical cord cysts are commonly classified as true cysts and pseudocysts. True cysts are rare, with a typical location near the fetal cord insertion. Allantoic cysts may resolve by themselves but may be associated with patent urachus, omphalocele, and possibly, obstructive uropathy.2 Pseudocysts may be associated with chromosomal anomalies, omphalocele, hemangiomas, and patent urachus.5 A higher risk of fetal anomalies is associated with the following: cyst detection in the second or third trimester, persistence of cysts after the first trimester, large size cysts, and cysts located near the fetal or placental end. Trisomy 18, 13, and 21 are also known to be associated, and in such cases, chromosomal analysis may be warranted.6
The pattern of limb shortening is assessed to determine which long-bone segments are more severely affected. There are four main patterns of shortening of the long bones: Rhizomelia—shortening of the proximal segment; Mesomelia—shortening of the middle segment [Figure 3]; Acromelia—shortening of the distal segment; and Micromelia— shortening of the entire limb. Rhizomelic and mesomelic dysplasia are encountered in cases of dwarfism, including many osteochondrodysplasias.7 Omphaloceles are associated with limb anomalies (rhizomelia, mesomelia, or acromelia) in syndromes like limb body wall complex, Cloacal exstrophy (OEIS) syndrome, and Trisomy 13, 18, and 21. However, based on previous studies, no specific/strong association could be found favoring the occurrence of one limb anomaly over another.
CONCLUSION
Once a prenatal diagnosis of an omphalocele is established and the defect and associated anomalies are characterized, prenatal counseling ensues to help the family determine the best course of action. If the patient elects to continue the pregnancy, a multidisciplinary team involving obstetrics, pediatric surgery, and neonatology should determine the best timing and route for delivery. Factors to consider when making these decisions include the defect size, organs exteriorized in the sac, the integrity of the membrane sac, and any other associated abnormalities.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent is not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil
Conflicts of interest
There are no conflicts of interest
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
REFERENCES
- Prenatal diagnosis and management of omphalocele. Semin Pediatr Surg. 2019;28:84-8.
- [CrossRef] [PubMed] [Google Scholar]
- Omphalocele secondary to spontaneous rupture of allantoic cyst in the third trimester of pregnancy. Case Rep Obstet Gynecol 2021:6940685.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomy and embryology of abdominal wall defects. Semin Pediatr Surg. 2022;31:151230.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis and management of beckwith-wiedemann syndrome. Front Pediatr. 2019;7:562.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Umbilical cord cysts: classification, diagnosis, prognosis, and pregnancy recommendations. Int J Gynecol Obstet. 2023;00:1-7.
- [Google Scholar]
- Placental and umbilical cord anomalies diagnosed by two- and three-dimensional ultrasound. Diagnostics. 2022;12:2810.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prenatal diagnosis of tibial hemimelia type I and omphalocele, a rare entity and postnatal correlation. BJR Case Rep. 2020;7:20200002.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]