Translate this page into:
Diagnostic importance of Bone scan and SPECT-CT in atypical cases of CRPS presenting to pain clinic: A case report
* Corresponding author: Suruchi Jain, Department of Nuclear Medicine, All India Institute of Medical Sciences, Bhopal, MP, India. jain.suruchi83@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Jain S, Jain S, Jain A, Singh D, Kumar P. Diagnostic importance of Bone scan and SPECT-CT in atypical cases of CRPS presenting to pain clinic: A case report. Future Health. 2024;2:74–77. doi: 10.25259/FH_19_2024
Abstract
Establishing a diagnosis of complex regional pain syndrome (CRPS) is challenging and often requires a multidisciplinary approach. Skeletal scintigraphy (bone scan) can be helpful in diagnosing and staging CRPS. Presented here is an interesting case of the right upper extremity and pectoral region pain, which upon evaluation with skeletal scintigraphy and single photon emission computed tomography with computed tomography (SPECT-CT) turned out to be Pancoast tumor.
Keywords
Complex regional pain syndrome (CRPS)
Pancoast tumor
skeletal scintigraphy
INTRODUCTION
Complex regional pain syndrome (CRPS) is difficult to diagnose and treat; mostly, the diagnosis is of exclusion. CRPS is characterized by swelling, pain, and raised temperature in the affected area. Usually, these changes follow an injury in the affected area. CRPS without an obvious antecedent injury is even more difficult to suspect.1 We are reporting a case where single-photon emission computed tomography with computed tomography (SPECT-CT) done along with bone scintigraphy provided evidence of a rare diagnosis, which ultimately changed the management plan.
CASE REPORT
A 61-year-old man, ex-smoker, presented to the pain clinic with the complaint of pain in the right upper limb for eight months. The pain had an insidious onset and was gradually progressive. Initially, the pain was severe during the night, but gradually it became persistent throughout the day. Pain in the scapular region and the arm was aching in nature, with an intensity of 7–8 on the numerical rating scale (NRS). There were occasional pin-prick sensations superimposed on the aching pain. The upper limb did not have any obvious swelling or color changes. There was no complaint of cough, fever, or chest pain. On palpation, there was mild tenderness in the anterior right upper hemithorax. There were no specific aggravating or relieving factors. Clinical examination was also inconclusive. He reported partial response (20–30% relief) to nonsteroidal antiinflammatory drugs (NSAIDs) and gabapentinoids.
Since the clinical findings were subtle, the pain physician considered the pain to be of musculoskeletal origin. Hence, the patient was referred for skeletal scintigraphy with SPECT/CT. A whole-body bone scan was performed after intravenous injection of Technetium-99m labeled with methylene diphosphonate (Tc99m-MDP), and SPECT-CT of the dorso-lumbar region was done. Bone scan revealed increased tracer uptake in the right shoulder, elbow, and small joints of the hand, along with higher uptake in the posterior aspect of the right first, second, and third ribs [Figures 1 and 2]. SPECT-CT scan of the high uptake region revealed a soft tissue mass in the upper lobe of the right lung with erosion of the overlying first, second, and third ribs [Figure 2]. A diffuse increased tracer uptake was also seen in all the bones of the right upper limb, including both long and small bones [Figures 1 and 3]. The findings were suspicious for the Pancoast tumor of the right lung with CRPS of the right upper limb. The possibility of bony metastasis was excluded on the basis of absent focal tracer uptake elsewhere on whole-body planar imaging.
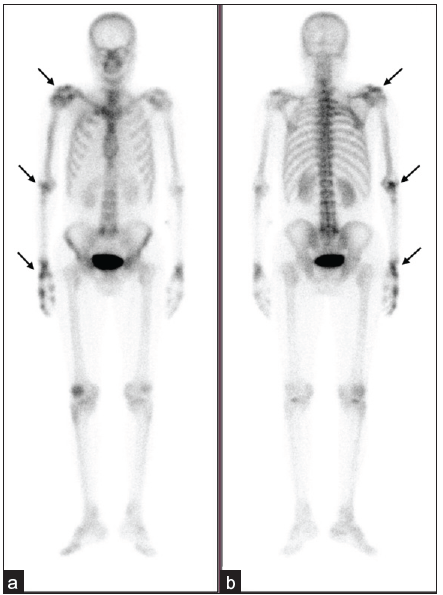
- Planar whole-body bone scintigraphy images acquired 3 hours after intravenous injection of Technetium-99m methylene diphosphonate (MDP) in (a) anterior and (b) posterior projections show increased tracer uptake in the right shoulder, elbow, and small joints of hands (arrows) and also mildly increased uptake in long bones of the right upper limb.
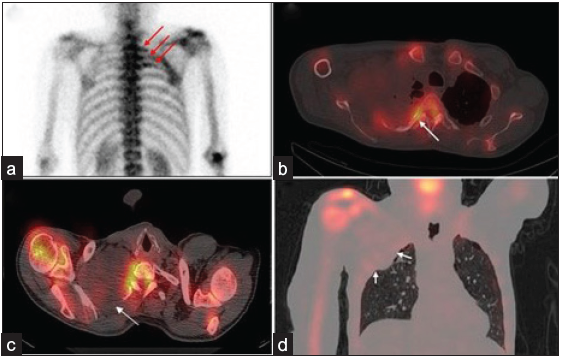
- (a) Posterior planar spot view of the thorax shows increased tracer uptake in the right 1st–3rd ribs (red arrows), which on Single Photon Emission Computed Tomography (SPECT/CT) images corresponds to erosion of these ribs (b) (arrow in axial bone window image, (c) by soft tissue mass in the upper lobe of the right lung (arrows in axial image (d) and arrows in the coronal lung window image).
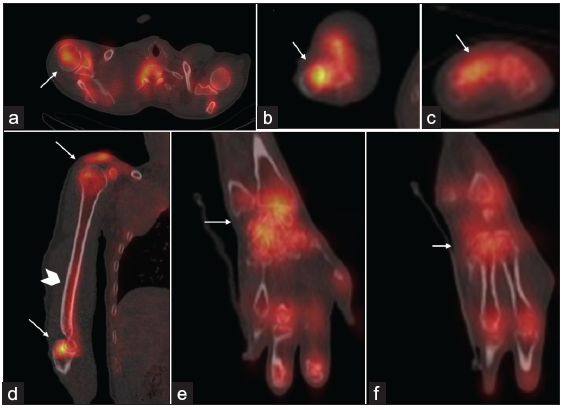
- (Arrows in a–f) Axial, sagittal, and coronal hybrid Single Photon Emission Computed Tomography (SPECT-CT) images of the right upper limb show increased tracer uptake in shoulder and elbow joints and peri-articular uptake in small joints of the hand. (Arrowhead in d) Diffusely increased tracer uptake is also noted in the right humerus.
The histopathological diagnosis of a malignant tumor mass in the apical region of the right lung was confirmed. The patient was referred to oncology services for treatment of the malignancy. For pain relief, the patient underwent an ultrasonography-guided stellate ganglion block, which provided excellent pain relief in the upper limb for about two weeks. Later, phenol neurolysis of the stellate ganglion was done, and the patient was pain free till the last available follow-up, which was done at eight weeks.
DISCUSSION
CRPS is a disorder characterized by sympathetically mediated pain, which is usually associated with swelling, stiffness, and skin changes in the affected area. CRPS is classified into two types based on the presence (CRPS-2) or absence (CRPS-1) of identifiable nerve lesions. Usually, all the four Budapest clinical criteria must be fulfilled to diagnose CRPS. All these findings may be present in the acute stage of CRPS,2 which usually lasts for one–three months. Over time, signs become less prominent, making the clinical diagnosis difficult.1,3
CRPS-1 in the setting of malignancy is infrequent; nevertheless, it has been reported in association with many malignancies, including gynecological malignancies (cervical, vulvar, and ovarian), Pancoast tumor,4 brain tumor, lymphoma, breast carcinoma, pancreatic carcinoma, urinary bladder carcinoma, and rarely hemagioendothelioma. CRPS, when present in malignant conditions usually involves the upper extremity.5 CRPS may present as a part of the paraneoplastic syndrome and precedes the appearance of typical symptoms of malignancy, while in some cases, CRPS may appear in the late stage of cancer due to the involvement of nerves by spreading local disease.6 When patients present with unexplained nontraumatic pain, primary bone tumor or metastasis is always considered as a differential. Like in this case, work up of patients for CRPS unravels underlying malignant conditions in many cases.
Skeletal scintigraphy is a useful tool to diagnose this condition as CRPS may exhibit different features in different phases of the disease. In the acute stage of the disease, scintigraphy characteristically shows an increased tracer flow and tracer pooling with a delayed articular and peri-articular uptake in small joints and larger joints. After that, tracer uptake in the early phase images may be normal but persistently increased in the delayed images. In the later stages of the disease (after 12–14 months), delayed phase uptake may return to normal, but perfusion and blood pool studies may show reduced tracer uptake.2 This case depicts imaging features of CRPS (stage two according to scintigraphy features) demonstrated by the increased uptake in the bones and small and large joints in the delayed images, without any abnormality in the perfusion and blood pool images.
The pooled sensitivity and specificity of bone scans in CRPS are estimated to be 80.4% and 85.3%, respectively.7 Local cytokine release (e.g., prostaglandin) results in increased vasodilation, which in turn increases the sensitivity and specificity of triple-phase bone scintigraphy.8 SPECT-CT enhances the specificity of findings noted on planar skeletal scintigraphy by delineating specific sites of tracer distribution and its correlation with anatomic changes. Skeletal scintigraphy also helps to exclude other diagnoses of extremity pain, such as arthritis, pseudo-arthropathy, and malignant etiology.9 Since the specificity of scintigraphy is modest, the diagnosis of CRPS needs to be confirmed with diagnostic sympathetic blocks. Functional recovery of CRPS depends on the stage at which specific treatment is initiated. Prognosis becomes less favorable with elapsing time, and untreated patients may become disabled for life.1,10 In this case, skeletal scintigraphy not only helped in diagnosing and staging CRPS when it was least suspected but also helped in identifying the Pancoast tumor. The data on the use of SPECT-CT in CRPS is scarce, and large prospective studies are required to validate its utility in diagnosis and implications on management.
CONCLUSION
Diagnosing CRPS is challenging and requires a multidisciplinary approach. Bone scintigraphy may be helpful when clinical signs are subtle. Incorporation of SPECT-CT findings may further help in management by delineating the etiology.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Complex regional pain syndrome: An updated comprehensive review. Neuro Rehabilitation. 2020;47:253-64.
- [CrossRef] [PubMed] [Google Scholar]
- Reflex sympathetic dystrophy: Diagnostic controversies. Semin Nucl Med. 1998;28:116-23.
- [CrossRef] [PubMed] [Google Scholar]
- Pancoast tumor as a cause of reflex sympathetic dystrophy. J Nucl Med. 1993;34:1992-4.
- [PubMed] [Google Scholar]
- Reflex sympathetic dystrophy as a probable paraneoplastic syndrome: Case report and literature review. Arthritis Rheum. 1984;27:1183-5.
- [CrossRef] [PubMed] [Google Scholar]
- Complex regional pain syndrome type I in cancer patients. Curr Rev Pain. 2000;4:227-33.
- [CrossRef] [PubMed] [Google Scholar]
- Usefulness of bone scintigraphy for the diagnosis of Complex Regional Pain Syndrome 1: A systematic review and Bayesian meta-analysis. PLoS One. 2017;12:1-18.
- [Google Scholar]
- The use of three-phase radionuclide bone scanning in the diagnosis of reflex sympathetic dystrophy. J Hand Surg Am. 1984;9:556-63.
- [CrossRef] [PubMed] [Google Scholar]
- Complex regional pain syndrome diagnosed with three-phase bone scan. J Nucl Med Technol. 2017;45:243-4.
- [CrossRef] [PubMed] [Google Scholar]
- Complex regional pain syndrome: practical diagnostic and treatment guidelines, 4th Edition. Pain Med. 2013;14:180-229.
- [CrossRef] [PubMed] [Google Scholar]







