Translate this page into:
A curious case of giant omental lipoma
*Corresponding author: Farhana Hasan, Junior Resident, Department of Radiodiagnosis, MGM Medical College and MY Hospital, Indore, MP, India. Farhana.hasan.0@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Shukla P, Hasan F. A curious case of giant omental lipoma. Future Health. 2024;2:69–73. doi: 10.25259/FH_9_2024
Abstract
Primary tumors of the omentum are one of the rare causes of large intra-abdominal masses and contribute to a limited number of reported cases in the medical literature. Here, we report a case of a male child with complaints of dull abdominal pain, suspected to be a giant omental lipoma radiologically, which was confirmed on histopathology after a complete surgical resection. The case highlights the importance of various radiological modalities for the diagnosis of omental lipomas and their importance in pre-operative workup to rule out malignant pathologies, and for better anatomical characterization of the lesion for assistance in surgical planning.
Keywords
Lipoma
Omentum
Liposarcoma
INTRODUCTION
Lipomas are the most common benign tumors of mesenchymal tissue and can occur virtually anywhere in the body where adipose tissue is present. Primary tumors of the omentum, let alone omental lipomas, are one of the rare causes of large intra-abdominal masses and contribute to a limited number of reported cases in the medical literature. 1 Giant omental lipomas, in adults, account for less than ten published cases reported worldwide. Omental lipoma in children is even rarer. Because of their infrequent occurrence, these cases may pose a diagnostic challenge. 2
CASE REPORT
A seven-year-old male child weighing 12 kg, presented with complaints of dull abdominal pain, fullness, and loss of appetite for six months. He had no other significant medical history.
Physical examination revealed a distended but non-tender, soft abdomen with no discrete mass palpable.
Abdominal ultrasound revealed a large, well-demarcated, homogeneous, solid, iso-to-hyperechoic intraperitoneal mass lesion measuring 6.2 × 22 × 19 cm (AP x Tr x CC), extending from epigastrium to hypogastrium and from right lumbar to the left lumbar region, displacing the bowel loops posteriorly [Figures 1a and 1b]. No vascularity was seen within. Giant omental lipoma was considered the probable diagnosis, with dermoid cyst, liposarcoma, and peritoneal mesothelioma as other possibilities.
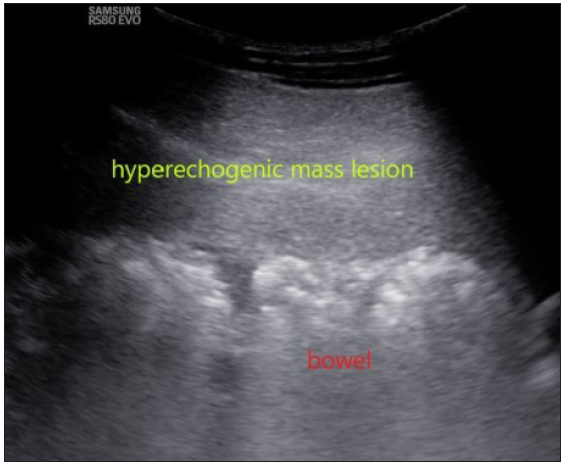
- Ultrasound showing a homogeneous echogenic solid mass lesion pushing the bowel loops posteriorly.
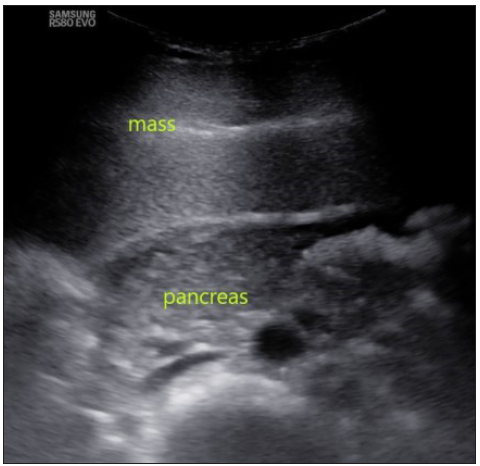
- In this ultrasound image, the mass is seen displacing the pancreas and major vessels posteriorly.
Contrast-enhanced computed tomography (CECT) abdomen was done, which showed a large diffuse fat attenuation (mean HU -100) intraperitoneal mass extending from epigastric region to pelvic cavity cranio-caudally and from right to left lumbar region, displacing the bowel loops posteriorly [Figures 2a–2f]. No internal calcifications, solid components, or septations were noted. On the post-contrast scan, there was no enhancement. No locally invasive features like the involvement of adjacent vasculature or bony erosion were noted. The primary diagnosis of giant omental lipoma was considered, with well-differentiated liposarcoma and mature cystic teratoma (dermoid cyst) as other possibilities.
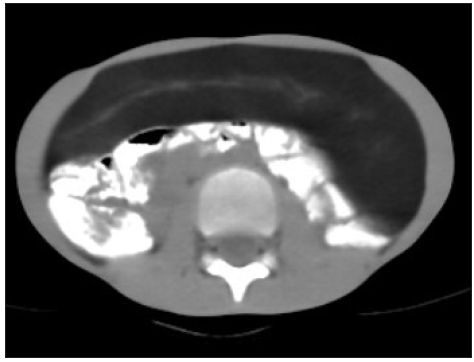
- Plain computed tomography (CT) axial section showing large well-defined intra-peritoneal diffuse hypo-attenuating lesion without calcifications.

- Arterial phase axial section showing no enhancement with hounsfield units (HU) of –97 indicating fat component.

- Post-contrast coronal section showing the craniocaudal extent of the lesion and displacement of the bowel loops.

- Post-contrast coronal section showing the pelvic extent of the mass.

- Post-contrast sagittal section.

- Post-contrast sagittal section showing the mass effect on bowel loops.
Magnetic resonance imaging (MRI) was not considered for further evaluation as it was unlikely to add any other useful information.
The case was discussed in a multidisciplinary team meeting (MDT), and consensus for curative surgical resection without prior biopsy was reached to avoid the risk of seeding in case the mass harbors any malignant foci. Surgeons went forward with lipoma or liposarcoma as probable diagnoses.
At laparotomy, the mass was confirmed to arise from the greater omentum, respecting its boundaries with adjacent vasculature and organs like the liver, spleen, and bowel loops. The mass was then excised in toto with a margin of macroscopically normal tissue.
Macroscopic examination revealed a large, well-defined, yellow, thinly encapsulated lipomatous mass measuring 7 × 27 × 22.5 cm in size and weighing 2.8 kg.
The patient was discharged once bowel function returned, and he became ambulatory. He was advised to three—six monthly follow-up CT scans.
On histopathology, mature adipocytes were present with focal areas of fat necrosis without atypical features or lipoblasts [Figures 3a and 3b]. These findings were consistent with an omental lipoma.
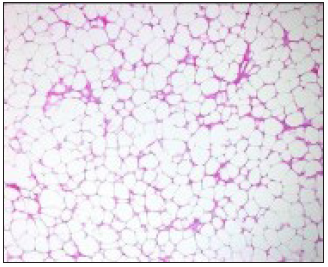
- Under low power, mature adipocytes are seen as relatively uniform in size and lacking cytological atypia.
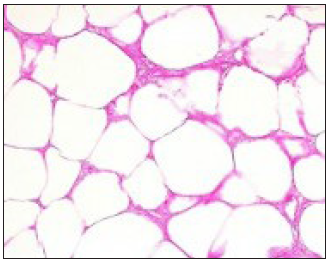
- Under high power (original magnification ×40), mature adipocytes are seen with focal areas of fibrosis and fat necrosis without atypical features or lipoblasts.
DISCUSSION
Lipomas are benign, well-encapsulated tumors comprised of mature adipocytes. They are among the most common mesenchymal tumors. 3 They can arise from any part of the body where adipose tissue is present, including subcutaneous tissues, extremities, the trunk, and rarely, intra-abdominal structures. Omental lipomas are extremely rare and limited to case reports in the literature. 3
A literature review performed by Cha, Jae Myung et al. 4 in 2007 showed that less than 30 cases of mesenteric lipomas were reported, with just seven cases in children. He presented a lipoma of 19 × 10 × 5.1 cm in a 29-year-old man and stated that this was one of the largest lipomas reported in the literature. 4
Usually, patients with omental lipomas are asymptomatic, but large lipomas can cause nonspecific symptoms. The symptoms are largely due to the mass effect of the lesion on adjacent structures and include abdominal pain, distention, early satiety, anorexia, vomiting, and constipation. Acute presentations typically reflect complications of torsion and infarction. 5
Ultrasound is the ideal first-choice modality for imaging, often providing excellent detail and resolution and allowing dynamic palpation and manipulation of the mass in real-time. CT further helps in mass characterization and better delineates the anatomical relationships with adjacent structures. 6 MRI can be considered in select cases, especially to rule out the malignant component, but it was not needed in this case.
The imaging findings of a lipoma at ultrasound, CT, and MRI are often diagnostic, thereby mitigating the need for further tests or, in some cases, even treatment. On ultrasound, lipomas are well-defined masses showing variable echogenicity, without posterior acoustic shadowing or enhancement, and sometimes with thin linear echogenic striations that parallel the skin. On CT, lipomas are encapsulated, homogeneous fat-attenuating masses with no soft-tissue component. At MRI, lipomas are isointense to subcutaneous fat on all sequences and also show loss of signal on fat suppression sequences. Thin septa (<2 mm) are frequently seen in lipomas. These septa typically demonstrate minimal or no enhancement. However, enhancing thickened or nodular septa have been reported in approximately one-third of benign lipomas and may have an appearance that is indistinguishable from liposarcoma. Lipomas may interdigitate with muscle fibers in the skeletal muscles and create a striated appearance that is not seen in liposarcomas. In general, the presence of thickened or nodular enhancing septa or enhancing soft-tissue components in a mass, showing fat attenuation on CT or fat signal intensity on MRI, should raise suspicion of liposarcoma. 7
Differential diagnoses in consideration include benign and malignant fat-containing pathologies, such as lipoma, liposarcoma, mature cystic teratoma, and peritoneal mesothelioma. 8 Sarcomas typically show some degree of solid component and enhancement and may show locally aggressive behavior in the form of invasion or infiltration of adjacent structures, depending on the grade of the tumor. Lipomas characteristically have a near-homogeneous fat composition, but differentiating liposarcoma from atypical lipomas can be challenging at times.
Lipomas may remain difficult to distinguish from well-differentiated liposarcomas radiologically. Fluorodeoxyglucose (FDG)-Positron Emission Tomography (PET) in these circumstances, generally reveals higher avidity in well-differentiated liposarcomas compared to lipomas. While histopathological diagnosis may be required in radiologically indistinguishable cases, core needle biopsy is controversial due to potential tumor cell seeding along the tract. 9
Peritoneal mesothelioma typically shows solid, heterogeneous, enhancing soft tissue mass along with the presence of calcified pleural plaques, indicative of asbestos exposure. Hence, in such cases, occupational history is very important. 10
The definitive treatment of omental lipomas is a complete surgical resection. In spite of their large size, they are usually easily removed due to their encapsulated nature and lack of local invasion. 6
Regular post-operative monitoring is recommended to ensure there is no recurrence, although the benign nature of lipomas typically indicates a low risk of recurrence of less than 5% after complete surgical excision. 11
CONCLUSION
Omental lipomas, although rare, should be considered a possibility for a fat-containing mass arising from the omentum or mesentery. Imaging is vital for the characterization and anatomy of the lesion, as well as to rule out any suspicious malignant areas within. The definitive management is surgery, which is usually only done in symptomatic cases, and complete surgical resection is achieved in most cases with a low rate of recurrence.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
REFERENCES
- Lipoma pathology. [Updated 2022 Dec 5] In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2023 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482343/
- [Google Scholar]
- Giant abdominal lipoma in adult. Case Rep Surg.. 2021;2021:6610533.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Omental lipoma: a rare cause of a giant intra-abdominal mass. J Surg Case Rep. 2022;2022:rjac160.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Giant mesenteric lipoma as an unusual cause of abdominal pain: a case report and a review of the literature. J Korean Med Sci.. 2009;24:333-6.
- [CrossRef] [PubMed] [Google Scholar]
- Giant omental lipoma, a rare etiology of right-iliac fossa pain in adult: A surgical case report. Int J Surg Case Rep. 2022;97:107428.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Imaging of abdominal wall masses, masslike lesions, and diffuse processes. Radiographics. 2020;40:684-706.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Imaging review of lipomatous musculoskeletal lesions. SICOT J.. 2017;3:34.
- [CrossRef] [PubMed] [Google Scholar]
- Increasing differential diagnosis between lipoma and liposarcoma through radiomics: a narrative review. Explor Target Antitumor Ther. 2023;4:498-510.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Radiomics approach to distinguish between well differentiated liposarcomas and lipomas on MRI. Br J Surg. 2019;106:1800-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Malignant peritoneal mesothelioma: a review. Ann Transl Med. 2017;5:236.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The recurrence of well-differentiated liposarcoma from benign giant intramuscular lipoma: A case (CARE-compliant) report. Medicine (Baltimore). 2021;100:e24711.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]







