Translate this page into:
Asymptomatic pulseless disease in upper limbs: An unusual presentation of ankylosing spondylitis
* Corresponding author: Dr. Vaibhav Yadav, M.D, Department of General Medicine, Mahatma Gandhi Memorial Medical College, Indore, Madhya Pradesh, India. vaibhav1125.90@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Pawar A, Yadav V, Joshi P. Asymptomatic pulseless disease in upper limbs: An unusual presentation of ankylosing spondylitis. Future Health. 2024;2:214-6. doi: 10.25259/FH_65_2024
Abstract
Ankylosing spondylitis (AS), a chronic inflammatory disorder of autoimmune etiology in young males, presents with inflammatory low back pain (axial skeleton) and human leukocyte antigen (HLA)-B27 positivity. Aorta and its branches involvement is associated with AS; however, it is uncommon. We present a case of HLA-B27 positive AS with involvement of major aortic branches, emphasizing the necessity of suspicion, clinical, and cardiovascular assessment in these individuals. To the best of our knowledge, there have been relatively few cases recorded from India and rest of the world.
Keywords
Ankylosing spondylitis
Autoimmune disease
Aortic arch syndrome
Rheumatology
INTRODUCTION
Ankylosing spondylitis (AS) is a chronic inflammatory condition with an autoimmune etiology that primarily affects the axial skeleton and peripheral joints, but rarely involves the aorta and its branches.1 Males are more prone to disease than females, it occurs more frequently in the second and third decades, and it has a strong association/correlation with human leukocyte antigen (HLA)-B27. Aortic arch syndromes are a group of illnesses that relate to a collection of signs and symptoms linked with structural abnormalities involving the aorta, aortic arch, and its branches via inflammatory and stenotic lesions with a variety of underlying etiologies.
Aorta and branch involvement is infrequent in AS, especially in men.1 We present a case of an 18-year-old male with HLA-B27 positive AS with asymptomatic left subclavian and left vertebral artery occlusion, emphasizing the importance of cardiovascular system examination and screening for early diagnosis, treatment, and prevention of its complications.
CASE REPORT
An 18-year-old boy presented to us with bilateral knee pain and swelling, ankle pain, hip joint pain, lower back pain, fever since 20 days, and no cutaneous, nails symptoms. He had been diagnosed with AS for the past eight years. He received 1 g of sulfasalazine twice a day and analgesics as needed. He couldn’t afford biological. He improved symptomatically with treatment in the early years, but later stopped follow-up and also stopped taking the medication on a regular basis. The patient also developed chronic uveitis as sequele to recurrent uvetis and was under the care of ophthalmologist since 2 years.
On inspection, there was no left radial or brachial artery pulse; there was no blood pressure recorded in the left upper limb, although it was 120/80 mm Hg in the right upper limb and 130/80 mm Hg in both lower limbs. The patient did not complain of any claudication, weakness, or wasting in any particular limb, nor did he have these symptoms in the past.
Further evaluation included an magnetic resonance imaging (MRI) of the bilateral pelvis with the sacroiliac joint, which revealed bilateral sacroiliitis [Figure 1]. The electrocardiogram (ECG) and two-dimensional (2D) echocardiography were normal, erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) was 22 mm/hr and 33 mg/L, respectively. The computed tomography (CT) aortogram revealed complete loss of flow enhancement and blockage in the whole left subclavian artery and left vertebral artery with collaterals [Figure 2]. X-rays of hands, feet, knee joint, and ankle joint were not suggestive of arthritic changes.
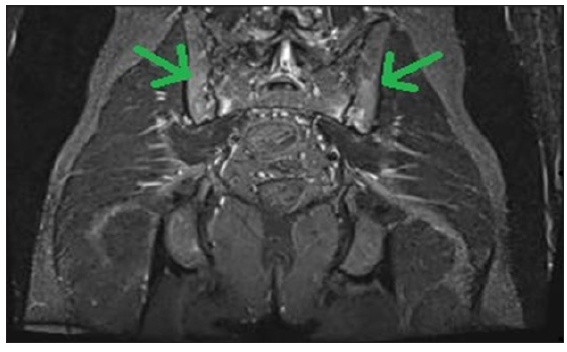
- Magnetic resonance imaging pelvis showing bilateral sacroiliitis (green arrows).
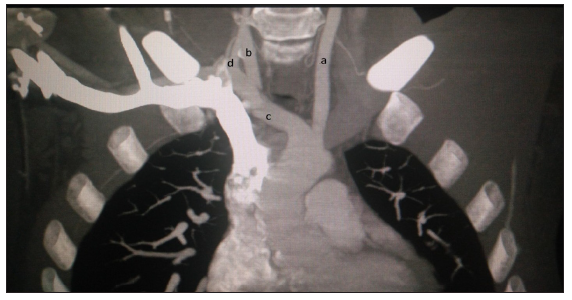
- Image of computed tomography aortogram showing—(a) Left common carotid artery, (b) Right common carotid artery, (c) Right subclavian artery, (d) Right vertebral artery; there is complete absence of flow in left subclavian artery.
DISCUSSION
The occurrence of cardiac symptoms in AS is widely documented, with the most prevalent being cardiac conduction abnormalities (atrioventricular [AV] blocks and intraventricular blocks). Aortic regurgitation (AR), aortitis, ischemic heart disease, peripheral vascular disease, and heart failure are also common disorders. The likelihood of these symptoms increases as the disease progresses. HLA-B27 is a greater risk factor for AS cardiac symptoms.2 In the past, a few occurrences of AS with involvement of the aorta and its branches were documented in various case reports, with many cases related with Takayasu arteritis and patients in either the older age group, female gender, or symptomatic.3 Patient has been diagnosed as non-radiological AS on the basis of MRI finding, suggestive of bilateral sacroiliitis along with clinical history and no significant finding on plain radiograph. As the patient does not have skin and nails manifestations, so the aortic involvement in this case is less likely due to psoriasis arthritis and more likely associated with AS. Patient’s symptoms of peripheral joint pain are not associated with arthritis of involved joint as X-rays were not suggestive of arthritic changes; so, similarly ankle joint pain is more likely due to enthesitis of Achilles tendon and to arthritic involvement of the ankle joint.
Previously, a similar case was reported by Balčiūnaitė et al. in 20204 who concluded that poor control of AS may speed up the development of serious cardiac vascular problems, which can also be the scenario in our reported case as patient has poor treatment compliance. One more article published by Hull et al. in 19841 also reported a similar case of AS with aortic arch syndrome.
Our patient is a young male with no clinical or radiological evidences of Takayasu arteritis and is asymptomatic regarding any feature of ischemia due to collaterals. It is important to examine/screen for any possible vascular involvement due to disease process and thus its early diagnosis, treatment, and prevention of complications.
CONCLUSION
Although aortic arch syndrome is infrequently related with AS, it is a devastating disorder with numerous consequences. With this case report, we intend to emphasize the importance of a complete clinical examination in patients with AS/chronic inflammatory autoimmune disorders with or without symptoms.
The involvement of the aorta and its branches in AS is a rare occurrence, especially after a long period of disease, but it has numerous early and late catastrophic problems that can be avoided. So, when treating a case of AS, we should consider a thorough general and cardiovascular examination as well as early screening for cardiovascular involvement in order to avoid numerous early and late significant sequelae.
Author contributions
VY: Concept and data collection; AP: Data collection and Review of literature; PJ: Manuscript writing and critical revisions
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing of the manuscript and no images were manipulated using AI.
REFERENCES
- Ankylosing spondylitis and an aortic arch syndrome. Br Heart J. 1984;51:663-5.
- [CrossRef] [PubMed] [Google Scholar]
- The risk of developing ankylosing spondylitis in HLA-B27 positive individuals. A comparison of relatives of spondylitis patients with the general population. Arthritis Rheum. 1984;27:241-9.
- [CrossRef] [PubMed] [Google Scholar]
- Takayasu’s arteritis and ankylosing spondylitis: Is it a fortuitous association? J Angiol Vasc Surg. 2020;5:1-5.
- [CrossRef] [Google Scholar]
- Ankylosing spondyloarthritis resulting severe aortic insufficiency and aortitis: Exacerbation of ankylosing spondyloarthritis and stenosis of the main left coronary artery after mechanical aortic valve implantation with cardiopulmonary bypass. Case Rep Rheumatol. 2020;2020:9538527.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]








