Translate this page into:
An exploratory cross-sectional study of awareness and barriers to adoption of telemedicine services among patients in Bangladesh
*Corresponding author: Dr. Samia Amin, Department of Public Health, Macquarie University, Sydney, Australia. drsamia27@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Amin S, Mustofa M, Rahman A, Barman H. An exploratory cross-sectional study of awareness and barriers to adoption of telemedicine services among patients in Bangladesh. Future Health. 2024;2:107-13. doi: 10.25259/FH_40_2024
Abstract
Objectives
Telemedicine has emerged as a promising solution to address healthcare challenges, particularly in resource-constrained settings such as Bangladesh. Understanding patient perspectives on telemedicine adoption is vital for improving healthcare delivery in such contexts.
Material and Methods
This cross-sectional study surveyed 120 patients in Bangladesh to explore awareness, acceptance, and barriers to telemedicine adoption. Data were collected using structured surveys administered face-to-face in 2024. Descriptive statistical techniques were employed for data analysis.
Results
Most respondents demonstrated awareness of telemedicine services, primarily learning about them through friends or online sources. They viewed telemedicine positively, especially for follow-up appointments and mental health services, expressing satisfaction with the services used. However, concerns regarding its effectiveness for emergency consultations were noted. Barriers to adoption included limited internet connectivity, trust/security issues, lack of awareness, regulatory challenges, and cultural resistance.
Conclusion
Despite positive attitudes towards telemedicine, challenges such as internet connectivity, trust concerns, and cultural barriers persist in Bangladesh. Addressing these challenges is essential for the successful implementation and widespread adoption of telemedicine, ultimately improving access to quality healthcare services. Future research should explore the perspectives of healthcare providers and policymakers and employ longitudinal and qualitative methods to gain deeper insights.
Keywords
Awareness
Barriers
Telemedicine
Patients
Bangladesh
INTRODUCTION
Telemedicine, defined as the remote diagnosis and treatment of patients using telecommunications technology, holds immense potential for improving healthcare outcomes1 particularly in resource-constrained settings such as Bangladesh.2,3 The advent of telemedicine has revolutionized healthcare delivery by leveraging technology to overcome geographical barriers and enhance patient access to medical services.2,4 Against the backdrop of a rapidly evolving healthcare landscape, understanding patient awareness, acceptance, and barriers to the adoption of telemedicine in Bangladesh is crucial for informing policy decisions and enhancing healthcare delivery.2-5
Bangladesh, a densely populated South Asian nation, faces numerous challenges in its healthcare system, including limited access to quality medical services, particularly in rural areas, and a shortage of healthcare professionals.6-8 In this context, telemedicine emerges as a promising solution to bridge the gap between healthcare supply and demand. Telemedicine initiatives in Bangladesh have gained momentum in recent years, facilitated by advancements in telecommunications infrastructure and the growing ubiquity of digital technologies.9
Bangladesh has developed telemedicine guidelines to streamline the use of telemedicine services, ensuring quality and consistency in telehealth practices. The Bangladesh Medical & Dental Council, under the Ministry of Health and Family Welfare, has been actively involved in formulating these guidelines, which include provisions for patient confidentiality, data security, and standards for telemedicine practices.10 These guidelines aim to promote the safe and effective use of telemedicine across the country. However, despite its potential benefits, the adoption of telemedicine in Bangladesh faces various challenges, ranging from technological barriers to cultural and regulatory hurdles.
There is a lack of comprehensive studies focusing on patient perspectives in Bangladesh, which is crucial for understanding the unique challenges and opportunities within this context. Addressing this gap is essential for developing tailored strategies that effectively promote the adoption and utilization of telemedicine services, ultimately improving healthcare access and outcomes in the region. Thus, this study seeks to explore the awareness, acceptance, and barriers to the adoption of telemedicine services among patients in Bangladesh. By examining patient perspectives, attitudes, and experiences related to telemedicine, this study aims to fill existing gaps in the literature and provide actionable insights for policymakers, healthcare providers, and other stakeholders. Understanding the factors influencing telemedicine adoption is critical for designing effective interventions, enhancing healthcare accessibility, and ultimately improving health outcomes in Bangladesh.
MATERIAL & METHODS
This study utilized a cross-sectional design, a widely employed method in public health research, to capture a snapshot of patient awareness and barriers to telemedicine adoption in Bangladesh. The study was conducted in a private clinic managed by a specialist doctor in Dhaka, Bangladesh, focusing on general healthcare services. The clinic is in an urban setting, catering to a diverse patient population that includes diverse age groups, genders, educational backgrounds, and socio-economic statuses to ensure a comprehensive understanding of factors influencing telemedicine adoption. Recruitment involved a convenience sampling approach, wherein patients visiting healthcare facilities were approached and invited to participate in the study. A sample size calculation was performed prior to the study to ensure sufficient power to detect significant differences and relationships. Based on a confidence level of 95%, a margin of error of 5%, and an assumed telemedicine awareness rate of 50%, the required sample size was determined to be 120 participants.
Formal ethics approval was not sought as the study involved minimal risk and collected anonymous, non-sensitive data in accordance with the ethical considerations for low-risk studies outlined by Wu et al. (2019).11 Informed consent was obtained from all participants, emphasizing voluntary participation, confidentiality, and the right to withdraw from the study at any time. To ensure privacy, data collection was conducted in private settings, and participant identifiers were anonymized during data entry.
Data collection was primarily conducted through structured surveys administered face-to-face by trained research assistants to maintain uniformity. The data collection period spanned 1 month, from March 2024. Efforts were made to ensure a diverse sample by including participants from different age groups, genders, educational backgrounds, and socio-economic statuses. The survey instrument was meticulously developed, utilizing validated measures from existing literature and tailored to the context of Bangladesh. It included sections for assessing participants’ demographic information, awareness of telemedicine services, acceptance, and perceived barriers to adoption.
Prior to implementation, the survey underwent pilot testing with 20 patients, who were randomly selected to ensure a representative sample of the larger population. The sample size of 20 was chosen based on standard practices for pilot testing, which recommend a small but enough to identify potential issues with the survey instrument without overextending resources. This testing aimed to assess clarity, comprehension, and relevance, with necessary modifications made based on feedback. Statistical measures, including Cronbach’s alpha, were used to evaluate internal consistency, yielding a Cronbach’s alpha value of 0.80, indicating good reliability. Based on feedback from the pilot test, necessary modifications were made to improve the survey instrument. These 20 patients were subsequently excluded from the main study.
Data analysis involved descriptive statistical techniques. Descriptive statistics, such as frequencies, means, and standard deviations, were used to summarize participant characteristics, levels of awareness, and perceived barriers. All analyses were conducted using SPSS statistical software (IBM SPSS Statistics for Windows, Version 27.0. Armonk, NY: IBM Corp).
RESULTS
The survey included 120 respondents from Bangladesh. The majority (35%) were in the age group of 46–55 years, followed by 36–45 years (21.7%) and 26–35 years (14.2%). A total of 54.2% of the respondents were male, and 45.8% were female. A significant portion (44.2%) had completed high school as their highest level of education. In terms of monthly income, 25.8% earned between 20,000 and 30,000 Bangladeshi Taka [Supplementary Table 1].
Telemedicine awareness
Awareness of telemedicine was assessed through direct survey questions asking respondents how they first learned about telemedicine services. A total of 35.8% of the respondents first learned about telemedicine services through friends or family recommendations, and 25.8% learned about it through online sources. Other sources included healthcare providers (15.9%) and media (10%). Despite a significant percentage having heard about telemedicine through various sources, 12.5% of the respondents had never heard of telemedicine prior to this study [Figure 1].

- Channels through which patients first became aware of telemedicine.
Survey respondents identified consultations with general practitioners (45%), follow-up appointments (30%), mental health services (21.7%), medication management (21.7%), and chronic disease management (15%) as suitable healthcare services to be provided through telemedicine, while 14.2% expressed having no idea about appropriate use cases for telemedicine [Figure 2].
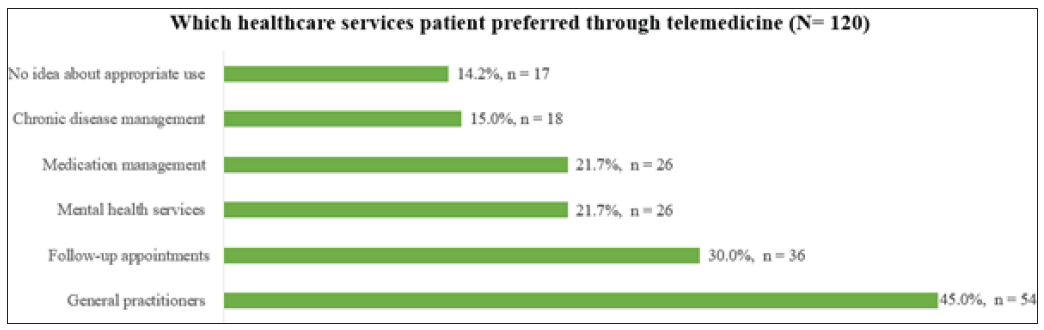
- Preferred healthcare services for telemedicine.
Telemedicine acceptance
Telemedicine acceptance was rated on a Likert scale, ranging from ‘Strongly Disagree’ to ‘Strongly Agree,’ with respondents indicating their level of agreement with the following statements on patients’ willingness to use telemedicine for various healthcare needs [Table 1]. The high rate of neutral responses, particularly regarding satisfaction with telemedicine services (82.5%), indicates a significant ambivalence among patients. This neutrality could be attributed to a lack of sufficient experience or information about telemedicine services. Such neutral stances highlight the need for more comprehensive education and exposure to telemedicine to foster informed opinions among patients.
| Strongly disagree | Disagree | Neutral | Agree | Strongly agree | |
|---|---|---|---|---|---|
| Telemedicine is a convenient alternative to traditional in-person healthcare services. | 2 (1.7%) | 13 (10.8%) | 58 (49.2%) | 38 (31.7%) | 8 (6.7%) |
| I feel satisfied with the telemedicine services I have used in Bangladesh. | 1 (0.8%) | 9 (7.5%) | 99 (82.5%) | 11 (9.2%) | 0 (0%) |
| Telemedicine is a suitable option for follow-up appointments. | 0 (0%) | 4 (3.3%) | 48 (40%) | 57 (47.5%) | 11 (9.2%) |
| I believe that telemedicine can effectively address mental health issues. | 0 (0%) | 11 (9.2%) | 74 (61.7%) | 31 (25.8%) | 4 (3.3%) |
| Telemedicine can provide standard emergency medical consultations. | 7 (5.8%) | 4 (3.3%) | 46 (38.3%) | 53 (44.2%) | 10 (8.3%) |
Participants’ views on the effectiveness of telemedicine for mental health issues were specifically assessed through a survey question asking them to rate their agreement with the statement ‘I believe that telemedicine can effectively address mental health issues’ [Table 1]. Most respondents (61.7%) were neutral about telemedicine’s effectiveness in addressing mental health issues, suggesting either uncertainty or insufficient experience. However, 25.8% saw it as effective, and 3.3% had a strong belief in its effectiveness. This indicated that while a portion of the population was open to the idea, more substantial evidence or experience may be needed to shift more opinions toward agreement.
The data showed a generally positive view towards telemedicine for emergency consultations, with 44.2% agreeing and 8.3% strongly agreeing on its suitability. However, 38.3% remained neutral, which could suggest either uncertainty or a need for more concrete evidence of its effectiveness in emergency situations. Around 9.1% were skeptical, reflecting concerns about the adequacy of remote consultations for urgent needs.
Barriers to telemedicine adoption
Perceived barriers to telemedicine adoption were assessed using a Likert scale, ranging from ‘Strongly Disagree’ to ‘Strongly Agree.’ Respondents were asked to indicate their level of agreement with the provided statements, such as challenges faced by patients in adopting telemedicine, such as internet connectivity, trust in the technology, and regulatory issues [Table 2].
| Strongly disagree | Disagree | Neutral | Agree | Strongly agree | |
|---|---|---|---|---|---|
| Limited internet connectivity is a significant barrier to the widespread adoption of telemedicine. | 0 (0%) | 2 (1.7%) | 57 (47.5%) | 42 (35%) | 19 (15.8%) |
| Trust and security concerns regarding telemedicine platforms hinder their adoption | 0 (0%) | 0 (0%) | 52 (43.3%) | 49 (40.8%) | 19 (15.8%) |
| Lack of awareness is a major obstacle to the acceptance of telemedicine in Bangladesh. | 0 (0%) | 1 (0.8%) | 51 (42.5%) | 29 (24.2%) | 39 (32.5%) |
| Regulatory issues are preventing the effective implementation of telemedicine. | 0 (0%) | 2 (1.7%) | 75 (62.5%) | 29 (24.2%) | 14 (11.7%) |
| Cultural resistance is a significant barrier to the acceptance of telemedicine in Bangladesh | 0 (0%) | 5 (4.2%) | 57 (47.5%) | 36 (30%) | 22 (18.3%) |
Most respondents (47.5%) were neutral regarding the impact of limited internet connectivity on telemedicine adoption. However, 35% agreed, and 15.8% strongly agreed that limited internet connectivity was a significant barrier. Only a small percentage of respondents (1.7%) disagreed with this view, indicating that while many recognized the issue, there was a range of opinions on its severity.
Many respondents (43.3%) were neutral about the role of trust and security concerns in hindering telemedicine adoption. Meanwhile, 40.8% agreed, and 15.8% strongly agreed that these concerns were significant obstacles. Notably, no respondents disagreed or strongly disagreed, suggesting a widespread recognition of trust and security issues as key barriers.
Respondents were quite divided on the impact of lack of awareness on telemedicine adoption. While 42.5% remained neutral, 24.2% agreed, and 32.5% strongly agreed that lack of awareness was a major obstacle. A very small percentage (0.8%) disagreed, highlighting that while awareness was seen as a challenge, there was considerable agreement on its importance.
Regarding regulatory issues, a large majority of respondents (62.5%) were neutral. However, 24.2% agreed, and 11.7% strongly agreed that regulatory issues were preventing the effective implementation of telemedicine. A small percentage (1.7%) disagreed, indicating that while regulatory challenges were recognized by some, there was a significant level of neutrality regarding their impact.
Cultural resistance was viewed with mixed opinions among respondents. A substantial portion (47.5%) were neutral, but 30% agreed and 18.3% strongly agreed that cultural resistance was a significant barrier to telemedicine acceptance. Only 4.2% disagreed, showing that while cultural resistance was recognized by many as a barrier, there were varying levels of agreement on its significance.
DISCUSSION
This study aimed to explore the awareness, acceptance, and barriers to the adoption of telemedicine services among patients in Bangladesh. The survey revealed several key findings. Firstly, a considerable proportion of respondents, particularly those in the age group of 46–55 years, demonstrated awareness of telemedicine services. However, it is noteworthy that a significant percentage had never heard of telemedicine, indicating a need for increased awareness campaigns. Furthermore, those who were aware of telemedicine generally agreed with most of the questions regarding its acceptance and potential benefits. This indicates that while there is a lack of awareness, there is also a positive perception among those familiar with telemedicine, suggesting a potential for higher acceptance with increased education and exposure. Secondly, most respondents viewed telemedicine positively, perceiving it as a convenient alternative to traditional healthcare services, particularly for follow-up appointments and mental health issues. The mixed opinion reflected a majority neutrality (61.7%) on telemedicine’s effectiveness for mental health, with some viewing it as effective (25.8%) and others strongly believing in its efficacy (3.3%), suggesting that while there is some openness to telemedicine, further research and experience may be needed to build stronger consensus and confidence in its role in mental health care. Additionally, most respondents expressed satisfaction with the telemedicine services they used. However, there were notable concerns regarding the effectiveness of telemedicine in providing standard emergency medical consultations, indicating a need for more evidence and reassurance regarding its effectiveness in urgent situations. Thirdly, perceived barriers to telemedicine adoption include limited internet connectivity, trust and security concerns regarding telemedicine platforms, lack of awareness, regulatory issues, and cultural resistance. Among these factors, trust and security concerns were identified as the primary barriers to telemedicine adoption. Additionally, lack of awareness and internet competitiveness was also a notable obstacle, while cultural resistance and regulatory issues were viewed as the least critical barrier.
Our study reveals that a significant proportion of respondents, particularly those aged 46–55 years, have some awareness of telemedicine services. However, a notable percentage of participants were unfamiliar with telemedicine, highlighting a crucial need for enhanced awareness campaigns. This finding is consistent with prior research emphasizing that awareness is a critical factor influencing telemedicine adoption.12-17 For example, Bali (2018) found that low awareness levels were a significant barrier to telemedicine uptake in developing countries.18 Our study corroborates this view, demonstrating that while there is a positive perception among those who are aware, the broad gap in awareness necessitates targeted educational initiatives to improve overall understanding and acceptance.
In terms of perception, our results show a generally positive view of telemedicine, with respondents appreciating its convenience for follow-up appointments and mental health issues. This finding aligns with Almasi et al. (2022), who reported that telemedicine is perceived favorably, particularly for non-urgent consultations.13 However, the mixed opinions regarding telemedicine’s effectiveness for mental health care—where some respondents remain neutral—reflect findings from prior literature that indicate the efficacy of telemedicine in mental health care is still debated.19,20 This skepticism suggests a need for further empirical research and clinical trials to build a stronger consensus on its effectiveness in mental health services. The mixed views highlight that, while there is openness to telemedicine, further evidence is necessary to enhance confidence in its broader applications.
Patients’ satisfaction with telemedicine services in this study mirrors findings from previous studies demonstrating high patient satisfaction with telemedicine consultations.19-23 The high levels of satisfaction expressed by respondents align with previous research, such as Kruse et al. (2017), who found high patient satisfaction with telemedicine, particularly regarding its convenience and accessibility.23 Nonetheless, concerns about telemedicine’s effectiveness for emergency consultations were prominent. This supports the conclusions of Hayden et al. (2023), who emphasized that while overall satisfaction is high,24 areas, such as emergency care, require more rigorous evaluation to ensure that telemedicine effectively meets all healthcare needs. This need for further evaluation underscores the importance of continually assessing and improving telemedicine services to address specific concerns and enhance overall effectiveness.
Our study identified several barriers to telemedicine adoption, with trust and security concerns emerging as the primary obstacle. This finding was consistent with research by Houser et al. (2023), who identified trust and security as significant impediments to telemedicine adoption.25 Limited internet connectivity and lack of awareness were also identified as major barriers, consistent with the Houser et al. (2023) study, which highlighted that inadequate infrastructure and knowledge gaps are critical challenges in developing regions.25
However, the emphasis on cultural resistance as a significant barrier in this study adds a unique dimension to the literature. While previous research has recognized cultural factors influencing healthcare utilization,26 our study underscores the specific cultural context of Bangladesh, where traditional healthcare practices and beliefs may impact the acceptance of telemedicine. This finding emphasizes the need for culturally tailored strategies to promote telemedicine acceptance and address cultural barriers effectively.
Regulatory issues were highlighted as a barrier, primarily in terms of the lack of clear policies and regulations governing telemedicine practices. Participants expressed concerns about the absence of standardized protocols, which hampers the effective implementation of telemedicine services. Moreover, the prevalence of regulatory issues hindering telemedicine implementation echoes findings from studies highlighting regulatory challenges as a barrier to telemedicine adoption in both developing and developed countries.27 Understanding and addressing these regulatory challenges are critical for creating an enabling environment for telemedicine services.
The strengths of this study lie in its diverse sample representation, patient-centric approach, quantitative assessment methods, and comprehensive examination of telemedicine-related factors. These strengths contribute to the robustness of the study’s findings and their potential applicability in informing telemedicine strategies and initiatives in Bangladesh and beyond. While a qualitative design could offer deeper insights into individual experiences and perceptions, the quantitative approach used here is effective for identifying general trends and patterns across a diverse population, which is essential for informing policy and large-scale interventions. This study has several limitations. Firstly, the survey relied on self-reported data, which may be subject to recall bias as respondents were asked to recall their experiences and perceptions regarding telemedicine, which could be influenced by recent events or interactions. Secondly, the study’s cross-sectional design limits the ability to establish causal relationships between variables. Additionally, the sample may not fully represent the entire population of Bangladesh, particularly those with limited access to healthcare services. Furthermore, the study did not account for patient-related factors (e.g., comorbidities, individual health behaviors, adherence to prescribed treatments or lifestyle choices), illness-related factors (e.g., disease stage, duration of illness, or previous treatments received), or facility-related factors (e.g., availability of specialized equipment, staff expertise, or differences between urban and rural healthcare settings), which limited the comprehensiveness and applicability of the findings.
Future research could explore the perspectives of healthcare providers and policymakers to gain a comprehensive understanding of the barriers and facilitators to telemedicine adoption in Bangladesh. Longitudinal studies could assess changes in awareness and acceptance of telemedicine over time. Moreover, qualitative research methods, such as interviews and focus groups, could provide deeper insights into the cultural factors influencing telemedicine utilization.
CONCLUSION
This study contributes to the growing body of literature on telemedicine adoption by shedding light on the current state of awareness, perceptions, and barriers among patients in Bangladesh. The findings align with prior research while offering new insights, particularly regarding cultural and regulatory factors. Addressing the identified barriers—such as increasing awareness, enhancing the evidence base for telemedicine’s effectiveness, and resolving trust, security, and regulatory issues—will be essential for improving telemedicine adoption. Continued research and tailored strategies will be crucial in overcoming these barriers and enhancing telemedicine services in similar contexts.
Ethical approval
Institutional Review Board approval is not required as the study involved minimal risk and non-sensitive data.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing of the manuscript and no images were manipulated using AI.
REFERENCES
- Telehealth: Defining 21st century care. Arlington, VA: ATA; 2020. [Last accessed 2024 June 01]. Available from: https://www.americantelemed.org/resource/why-telemedicine/
- Telehealth benefits and barriers. J Nurse Pract. 2021;17:218-21.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Telemedicine in low- and middle-income countries during the COVID-19 pandemic: A scoping review. Front Public Health. 2022;10:10.
- [CrossRef] [Google Scholar]
- Telemedicine for healthcare: capabilities, features, barriers, and applications. Sens Int. 2021;2:100117.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Expectations of telemedicine health service adoption in rural Bangladesh. Soc Sci Med. 2019;238:112485.
- [CrossRef] [PubMed] [Google Scholar]
- Health system challenges and opportunities in organizing non-communicable diseases services delivery at primary healthcare level in Bangladesh: A qualitative study. Front Public Health. 2022;10:1015245.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- World population review Bangladesh population 2023. 2023. [Last accessed 2024 June 01]. Available from: https://worldpopulationreview.com/countries/bangladesh-population
- The health workforce crisis in Bangladesh: Shortage, inappropriate skill-mix and inequitable distribution. Hum Resour Health. 2011;9:9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Use of telemedicine in Bangladesh: Current status and future prospects. North American Acad Res. 2022;5:1-13. Available from: https://doi.org/10.5281/zenodo.6407570
- [Google Scholar]
- Bangladesh Medical & Dental Council, Telemedicine guideline 2020 [Last accessed 2024 June 01]. Available from: https://www.bmdc.org.bd/docs/BMDC_Telemedicine_Guidelines_July2020.pdf
- Reporting of ethical approval and informed consent in clinical research published in leading nursing journals: A retrospective observational study. BMC Med Ethics. 2019;20:94.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The empirical evidence for telemedicine interventions in mental disorders. Telemed J E Health. 2016;22:87-113.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Efficacy of telemedicine for the management of asthma: A systematic review. Tanaffos. 2022;21:132-45.
- [PubMed] [PubMed Central] [Google Scholar]
- The impact of medical teleconsultations on general practitioner-patient communication during COVID- 19: A case study from Poland. PLoS One. 2021;16:e0254960.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A longitudinal qualitative study of the UK general practice workforce experience of COVID-19. Prim Health Care Res Dev.. 2022;23:e45.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Factors influencing adoption and use of telemedicine services in rural areas of China: Mixed methods study. JMIR Public Health Surveill.. 2022;8:e40771.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Barriers to development of telemedicine in developing countries. Telehealth. IntechOpen 2019. Available from: http://dx.doi.org/10.5772/intechopen.81723
- Tele-medicine and improvement of mental health problems in COVID-19 pandemic: A systematic review. Int J Methods Psychiatr Res. 2022;31:e1924.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Psychiatric treatment conducted via telemedicine versus in-person modality in posttraumatic stress disorder, mood disorders, and anxiety disorders: Systematic review and meta-analysis. JMIR Mental Health. 2023;10:e44790. Available from: https://doi.org/10.2196/44790
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The development of evaluation scale of the patient satisfaction with telemedicine: A systematic review. BMC Med Inform Decis Mak. 2024;24:31.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Patient satisfaction with telehealth at an academic medical center primary care clinic. Telemed J E Health. 2024;30:103-7.
- [CrossRef] [PubMed] [Google Scholar]
- Telehealth and patient satisfaction: A systematic review and narrative analysis. BMJ Open. 2017;7:e016242.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Telehealth in emergency medicine: A consensus conference to map the intersection of telehealth and emergency medicine. Acad Emerg Med. 2021;28:1452-74.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Privacy and security risk factors related to telehealth services - A systematic review. Perspect Health Inf Manag. 2023;20:1f.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Health care and nursing in Saudi Arabia. Int Nurs Rev. 2008;55:125-8.
- [CrossRef] [PubMed] [Google Scholar]
- Healthcare professionals’ organisational barriers to health information technologies-a literature review. Int J Med Inform. 2011;80:849-62.
- [CrossRef] [PubMed] [Google Scholar]