Azygous anterior cerebral artery thrombosis causing bifrontal infarcts with abnormal behavior
Corresponding author: Dr Amit Kumar Kumar Paliwal (MD Radiodiagnosis) Department of Radiodiagnosis & Imaging, Military Hospital, Bhopal, Madhya Pradesh, India. amit_paliwal82@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Paliwal AK, Mishra A. Azygous anterior cerebral artery thrombosis causing bifrontal infarcts with abnormal behavior. Future Health. 2024;2:87–89. doi: 10.25259/FH_2_2024
Abstract
Azygous anterior cerebral artery (AACA) is a rare anatomical variant and its occlusion may cause bifrontal infarct with variable neurological deficit and clinical presentation. In our case AACA thrombotic occlusion caused bifrontal infarcts leading to abnormal behavior. Early imaging with CT angiography or MRI with MRA is the key for early diagnosis and prompt management.
Keywords
Azygous Anterior Cerebral Artery
Bifrontal Infarct
MRI
MRA
INTRODUCTION
Azygous anterior cerebral artery (AACA) is a rare anatomical variant.1 Anterior cerebral artery supplies the anteromedial part of bilateral frontal lobes, and it’s occlusion may cause acute infarction in its territory.2 We present the case of a young male, who presented with abnormal behavior secondary to bifrontal infarction due to thrombotic occlusion of AACA.
CASE REPORT
A 36-year-old male without any previous comorbidities was brought to the hospital due to abnormal behavior since waking up in the morning. On examination, there was loss of insight, but no motor or sensory neurological deficit was present. Urgent MRI (magnetic resonance imaging) brain with MRA (magnetic resonance angiography) was done, which showed restricted diffusion on diffusion-weighted images (DWI) and corresponding apparent diffusion coefficient (ADC) maps in medial frontal lobes (right>left) bilaterally [Figure 1]. These areas were unremarkable on T1 weighted, T2 weighted, and Fluid attenuated inversion recovery (FLAIR) sequences. Also, MRA showed right hypoplastic A1 and normal sized left A1 fusing to form a single midline vessel with no division suggestive of AACA with occlusion just distal to the origin of the callso-marginal artery that is the beginning of the A3 segment [Figures 2, 3–4].
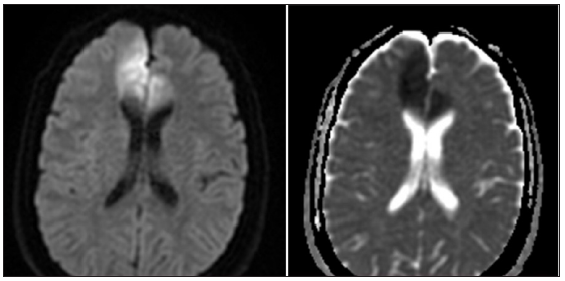
- Restricted diffusion on diffusion-weighted images (DWI) and corresponding apparent diffusion coefficient (ADC) maps in medial frontal lobes bilaterally (right>left).

- Magnetic resonance angiography (MRA): coronal Multiplanar reformation (MPR) showing right hypoplastic A1 and normal sized left A1 fusing to form a single midline vessel with no division suggestive of Azygos anterior cerebral artery (AACA) with occlusion at beginning of A3 segment.
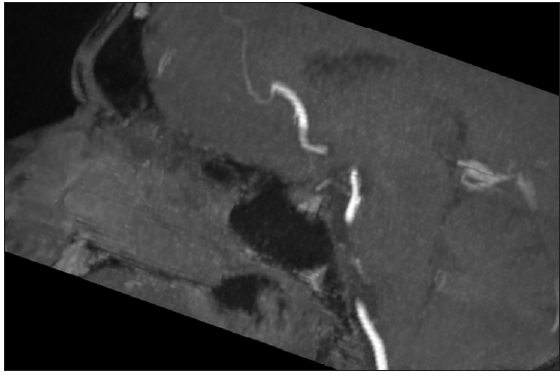
- Magnetic resonance angiography (MRA): Sagittal multiplanar reformation (MPR) showing Azygos anterior cerebral artery (AACA) with occlusion just distal to origin of callso-marginal artery i.e beginning of A3 segment.

- Magnetic resonance angiography (MRA): Volume Rendering Technique (VRT) image showing single midline vessel with no division suggestive of Azygos anterior cerebral artery (AACA) with occlusion at beginning of A3 segment.
Thus, a diagnosis of thrombotic occlusion of AACA with associated acute ischemic infracts was made. The patient was managed conservatively with anticoagulants. Evaluation revealed hypertriglyceridemia (Serum triglyceride: 342 mg/dl), rest of the prothrombotic workup was negative. Patient behavioral changes improved over time and at present (after eight months) except for some forgetfulness, patient is asymptomatic.
DISCUSSION
Anterior cerebral artery (ACA) has been divided classically into five segments, namely, one pre communicating segment (A1) and four post communicating segments—infracallosal (A2), precallosal (A3), supracallosal (A4), and posterocallosal (A5) segments. It has varied territory and mainly perfuses medial frontal lobes and the anterior part of the corpus callosum.3 ACA and its branches exhibit many variants which may be clinically significant or incidental. AACA is a rare variant where two A2 segments fuse to form a single midline vessel.1–4 Another similar variant is bihemispheric ACA, in which one A2 segment is hypoplastic (or terminates early), and the contralateral A2 segment divides to supply both hemispheres.2–4 AACA is associated with saccular aneurysms5 and midline facial and brain abnormalities, including holoprosencephaly, dysgenesis of the corpus callosum, and porencephalic cyst.6 Rarely bihemispheric infarcts, may occur due to occlusion of AACA.2,7
ACA infarcts are rare, and bilateral ACA occlusion-causing bihemispheric infarcts have been reported very rarely.2,7,8
Only a few case reports are available wherein AACA occlusion causing bihemispheric infarcts has been demonstrated. Fernando et al.2 reported a case of occlusion of AACA in a 45-year-old woman presenting with sudden-onset weakness in all four limbs. de Sousa CS et al.7 reported occlusion of AACA with bifrontal infarcts on CT angiogram in a 63-year-old diabetic and hypertensive patient with the sudden lowering of the level of consciousness. Khaliq et al.9 reported the case of a 50-year-old male patient with severe headache, dysarthria, and weakness in lower limbs with CT demonstrating occlusion of AACA with bifrontal infarcts.
In our case, the patient was a 36-year-old healthy male without any comorbidities, who presented with abnormal behavior, and MRI brain and MRA demonstrated AACA with occlusion at the origin of the A3 segment leading to bifrontal infracts. Association of AACA occlusion with bifrontal infracts causing abnormal behavior and its early diagnosis using MRI and MRA for diagnosis of this condition has been documented rarely. MRI offers early detection of infarcts and MRA offers excellent demonstration of vascular anatomy and occlusion as compared to CT and CT angiography, wherein the patient is exposed to ionizing radiation and to iodinated contrast. The disadvantage of using MRI is that it is costly and more time is required for scanning.
It is evident from all the case reports that bifrontal infarcts due to occlusion of AACA are rare, with varying clinical manifestations, and are difficult to diagnose clinically. Imaging using a CT scan with CT angiography or MRI with MRA is essential for early diagnosis and management of this condition.
CONCLUSION
AACA is a rare variant, and it’s occlusion may cause bifrontal infracts with variable neurological deficits and clinical presentation. Early imaging with CT angiography or MRI with MRA is the key to early diagnosis and optimal management.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent is not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Surgical neuro-angiography. Vol 1. Berlin: Springer; 2006. [Google Scholar]
- Azygous anterior cerebral artery infarction. Pract Neurol 2023:2023-003955. Epub ahead of print
- [Google Scholar]
- Anterior Cerebral artery: variant anatomy and pathology. J Vasc Interv Neurol. 2019;10:16-22.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Review of the Anatomy of the distal anterior cerebral artery and its anomalies. Turk Neurosurg. 2016;26:653-61.14294-15.1.
- [CrossRef] [PubMed] [Google Scholar]
- Saccular aneurysm of the azygos anterior cerebral artery: three case reports. J Korean Neurosurg Soc. 2007;42:342345.
- [Google Scholar]
- Persistent primitive olfactory artery: MR angiographic diagnosis. Surg Radiologic Anat. 2011;33:197-201.
- [Google Scholar]
- Thrombosis of the azygos anterior cerebral artery. Case Rep Radiol 2017:5409430.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Anterior cerebral artery territory infarction in the lausanne stroke registry. Clinical and etiologic patterns. Arch Neurol. 1990;47:144-50.
- [CrossRef] [PubMed] [Google Scholar]
- “Azygos anterior cerebral artery causing Bifrontal infarcts: a case report,”. Pakistan Journal of Neurological Sciences (PJNS). 2018;13 Article 6
- [Google Scholar]







